|
Roughly one in ten people who menstruate are affected by polycystic ovary syndrome (or polycystic ovarian syndrome) — better known as PCOS. To put that into perspective, the statistic adds up to more than 100 million individuals worldwide. If you fall into this category, perhaps you’ve noticed that PCOS impacts your sleep quality — and research confirms that PCOS and sleep have a close connection.
Since irregular cycles are a common feature of PCOS, it can be difficult to predict exactly when it might affect your sleep. Oura’s Cycle Insights feature can help you determine when your periods are due and make lifestyle adjustments to support better sleep — whether that’s going to bed a little earlier or clearing a busy schedule so you can get some rest.
READ MORE: How to Use Oura Temperature Trends to Track Your Cycle
Symptoms of PCOS
PCOS is the most common endocrine condition among women of childbearing age (roughly 15 to 45 years old). While everyone experiences it differently, there are three main symptoms used as reference points for diagnosis:
- Irregular periods: This occurs when the length of your menstrual cycle keeps changing because the eggs are not released regularly.
- Secretion of excess androgens: You might find you have a prevalence of body or facial hair, acne, high blood pressure, or hair loss.
- Polycystic ovaries: This is when your ovaries have become enlarged and contain many fluid-filled sacs.
Despite the fact that women with PCOS are 50% more likely to experience disturbed sleep than those without, this symptom is often overlooked both by professionals and patients. This may be because there are so many factors that contribute to it, including lifestyle, diet, illness, and stress.
Stress is another major contributor to sleep disorders. You can gain insights into your stress levels by checking your Readiness Score in your Oura App. There, you’ll find various Readiness Contributors, including heart rate variability (HRV). If your HRV is lower than your usual average, it could be an indicator of stress. Taking steps to manage your stress — for example, using guided meditations or breathing exercises — may help you get a better night’s sleep.
READ MORE: Try Oura’s Guided Meditations for Deep and Restful Sleep
How Does PCOS Affect Sleep?
While the cause of PCOS is unknown, according to PubMed, researchers believe there are several aspects of the condition that may aggravate sleep disorders, such as insomnia and sleep apnea. Below are some potential ways that PCOS may be contributing to your sleep disturbances.
READ MORE: Sleep Apnea, Defined — and How to Treat It
Hormonal Imbalances
Hormonal abnormalities are a common characteristic of PCOS. For instance, increased testosterone levels (hyperandrogenism) are responsible for the physical symptoms mentioned above.
PCOS also causes low levels of certain hormones like melatonin, which can wreak havoc on your body. Low melatonin levels can contribute to tiredness, sleep deprivation, and sleep apnea. Additionally, insufficient progesterone — a hormone that helps induce sleep — may make it harder to fall asleep.
Don’t worry. Below are some ways you can get your body feeling back to normal.
- A diet that’s high in carbohydrates can make insulin levels even higher, which can contribute to hormonal imbalances. Try to limit your intake of these foods and switch out for an alternative where possible.
- Be active. Exercise can lower your blood sugar levels while also helping you maintain a healthy weight.
- Do something that helps you calm down, like stretching or yoga. When you feel stressed, cortisol is released, which can worsen PCOS symptoms.
Use the Tags feature in the Oura App to monitor how your diet, lifestyle, and stress levels affect your PCOS symptoms. Over time, patterns may emerge that help you see what supports your body and what makes your symptoms worse.
If you need further support, don’t be afraid to seek guidance, support, and comfort elsewhere. A conversation with an endocrinology specialist or a gynecologist could ease some of your worries, and you can work together to address your most concerning symptoms.
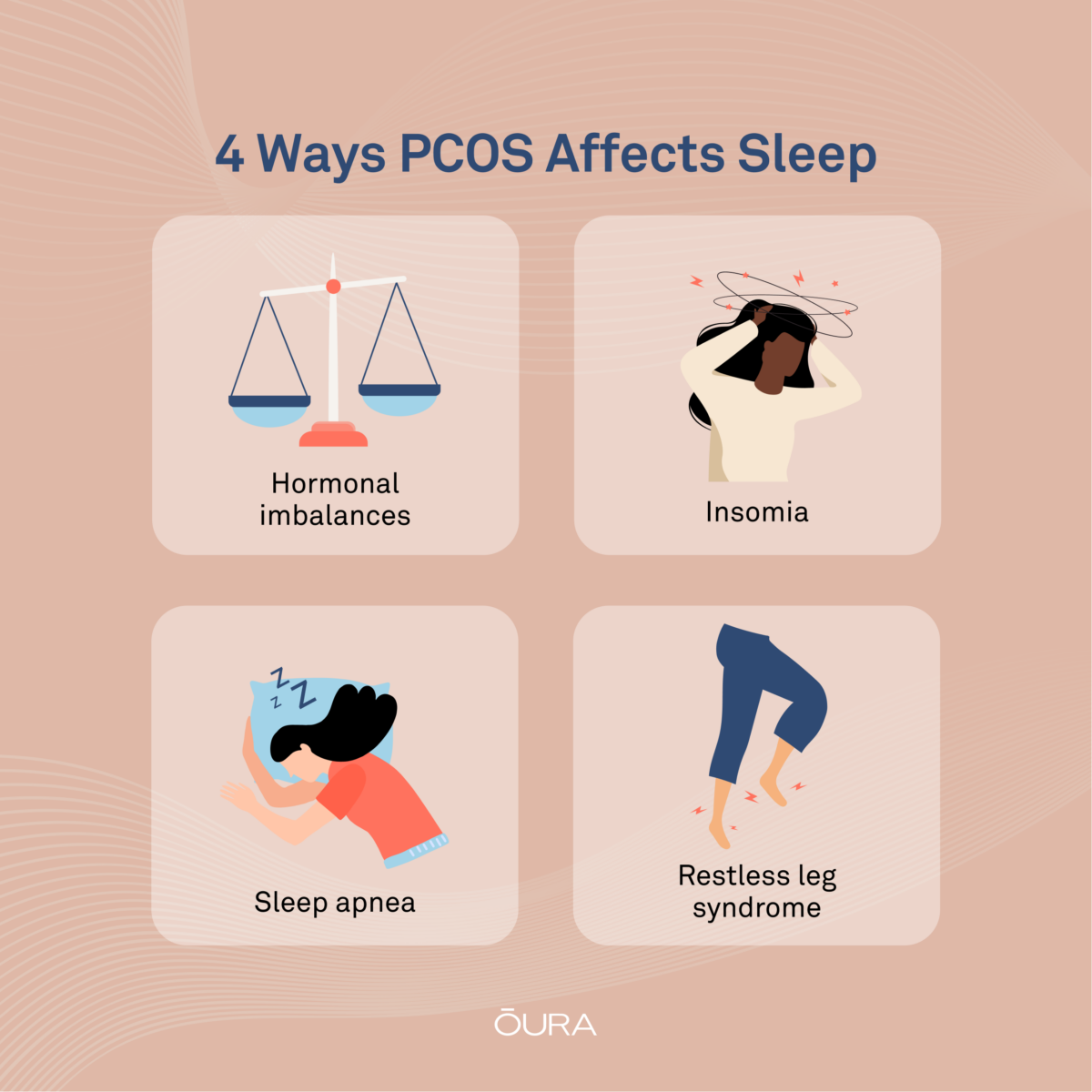
Insomnia and PCOS
Insomnia is characterized by either not being able to stay asleep or not sleeping at all. As you can imagine, this leads to problems like daytime sleepiness, difficulty concentrating, irritability, and in some cases, comorbidities like heart disease.
READ MORE: 4 Ways Sleep Affects Your Heart Health
Clinical studies have shown that insomnia happens more frequently in PCOS sufferers than in those who don’t have it. There are several causes for this, including hormone disruption and insulin resistance.
The good news is that, with the right care, insomnia is usually treatable without the need for sleep meds. Here are some methods to consider trying.
- Attempt to go to bed and wake up around the same time each morning. This will make it easier for your body to identify night from day, regulating your circadian rhythm. Finding a regular bedtime may help ease your insomnia by signaling your body to fall asleep at the same time each night. Oura’s Bedtime Guidance feature can recommend the optimal bedtime for your unique circadian rhythm.
- Try journaling before you close your eyes. This can be done in a notebook or in the notes app of your phone (although we recommend avoiding screen light before bed). Writing down your worries and to-do lists will prevent them from keeping you awake all night.
- Create the right environment. This will be different for everyone, but it may mean calming sounds, an audiobook, or earplugs.
Check the Trends tab in your Oura App to keep an eye on your bedtime and Sleep Contributors as you make these adjustments to identify what actions have the biggest impact on your sleep.
RELATED: Can PMS Affect Your Sleep Quality and Cause Insomnia?
Sleep Apnea and PCOS
Another common sleep disturbance for PCOS patients is obstructive sleep apnea (OSA). This occurs when the muscles that support the soft tissues in your throat relax, interrupting your normal breathing. This can result in excessive daytime sleepiness, morning headaches, irritability, snoring, and waking up with a sore throat.
It might be hard to imagine that the two are linked, but a cohort study has shown that the probability of sleep apnea is higher for those who have PCOS. Also, sleep apnea can exacerbate PCOS symptoms, including weight retention and hypertension.
It’s not all bad news, though. Dr. Esra Tasali, Director of the University of Chicago Sleep Center, found that treating OSA also improves PCOS symptoms. With that in mind, below are some remedies suggested by doctors.
- Consider continuous positive airway pressure (CPAP) therapy. The machine looks like a mask that delivers steady air pressure. To purchase one, you will need a prescription from your doctor or a sleep specialist.
- Use a humidifier to add moisture to the air. This will decrease congestion and open up your airways for easier breathing.
- One of the best ways to ease sleep apnea is to align your spine. Investing in an angled pillow will do just that whilst also preventing neck and back pain.
Worried you might have sleep apnea but don’t know for sure? Oura now offers Blood Oxygen Sensing (SpO2), which analyzes your blood oxygen levels and breathing regularity throughout the night. If your blood oxygen drops below 95% or irregularities are detected, it may be a sign of sleep apnea.

Restless Leg Syndrome and PCOS
Restless leg syndrome (RLS) affects your nervous system and can be very difficult to live with. Most people’s symptoms, which include the urge to move your legs and sensations such as prickling or itching, become worse at night. Naturally, this affects sleep duration, quality, and daytime sleepiness. Studies have shown that the hormonal imbalances that characterize PCOS may contribute to RLS.
Here are some of our top tips for finding that much-needed comfort when dealing with RLS.
- Engage in regular exercise. Movement during the day may ease the symptoms and distract you from any discomfort. Aim for around 20-30 minutes of moderate exercise each day. Good examples would be a walk, swimming, or yoga. Use Oura’s Cycle Insights feature to sync your training to your cycle for optimum results, and read more about how to align your training with your menstrual cycle here.
- The risk of metabolic syndrome is 11 times higher in women with PCOS. This can cause obesity, which can increase the likelihood of restless leg syndrome. It’s best to monitor your body mass index (BMI), cholesterol, and glucose levels and make sure they remain healthy.
- Make some dietary changes. A common cause of the condition is low iron, so eating things like spinach, red meat, and whole grains might ease the flare-ups. It has also been shown that avoiding large meals before bed helps you sleep better.
If RLS is keeping you up at night, use Oura’s helpful and friendly Movement Graph to monitor your nighttime movements and decide when to seek further advice from a healthcare professional.

Sleep Hygiene and PCOS
When someone says the words “sleep hygiene,” it might conjure up an image of washing your bedsheets and putting on clean pajamas. That isn’t quite what we’re talking about here. The term refers to the behavioral and environmental practices that can help you get the most consistent and fulfilling snooze possible.
RELATED: 5 Ways to Upgrade Your Sleep Hygiene
Achieving healthy sleep can improve your physical well-being, reduce your stress levels, and increase your overall quality of life. This might sound like it will be easier said than done, but below, you’ll find our tried-and-tested best practices for good sleep hygiene.
- Avoid caffeinated or alcoholic beverages in the evenings.
- Establish a relaxing and repeatable bedtime routine. Try journaling, reading, taking a nice warm bubble bath, lighting a few candles, or practicing breathing techniques.
- Blue light is not your friend. A scroll on social media is fun, but it can seriously affect your ability to sleep. Switch off electronics at least an hour before bed.
READ MORE: How Blue Light Affects Your Sleep
Your Journey To A Good Night’s Sleep Begins with Oura
Finding what best helps you manage your PCOS symptoms and sleep disturbances will take time and patience. However, with Oura’s personalized insights and recommendations, you can make the journey shorter.
Oura is committed to prioritizing women’s health, and we aim to empower you with all the knowledge you need to make the right decisions for your reproductive health. Find out more about how your Oura data can help you understand your menstrual cycle here.











