Pregnancy is a marathon, not a sprint. Like any marathon, it’s helpful to train your body to build strength, resilience, and endurance for the big race—the birth and parenting!
Hitting the gym might feel like the last thing you want to do if you’re struggling with morning sickness or swollen feet, but research suggests it has major upsides. From reducing anxiety, stress, and depression to improving birth outcomes and accelerating postpartum recovery, exercise plays an essential role during pregnancy and beyond.
Below, discover the benefits of exercise during pregnancy, what types of workouts might be best, and how to adjust your exercise trimester-by-trimester.
| Member Tip: Oura’s newly updated Pregnancy Insights feature supports mothers-to-be with data-backed insights, support, and education throughout every phase of their journey. |
Why Exercise Matters During Pregnancy
According to the American College of Obstetricians and Gynecologists (ACOG), staying active can reduce the risk of gestational diabetes, preterm birth, preeclampsia, and even cesarean sections.
To name a few more bonuses: It can also boost your mood, improve sleep quality, enhance stamina for labor and delivery (remember, it’s like a marathon!), build habits that will guide you postpartum, and increase your energy levels throughout, all while alleviating common discomforts like back pain and fatigue.
READ MORE: The Most Effective Coffee Alternatives for Pregnancy
How Much Exercise Should You Do in Pregnancy?
The ACOG recommends:
- Aim for about 150 minutes of moderate aerobic activity per week, such as brisk walking, swimming, or cycling. This equates to about 30 minutes a day, five days a week. Shorter sessions spread throughout the day also work if that feels more manageable.
- If you’re new to movement, start slow—even 5–10 minutes a day can make a difference, and you can build up gradually over time.
- If you’re already active, you can likely stick with your usual routine—with your provider’s approval. Just be sure to listen closely to your body and fuel accordingly.
- Exercise output can remain stable across trimesters, but intensity, positioning, and duration should be adjusted, especially in the third trimester when changes in balance, energy levels, and joint laxity become more pronounced.
- Focus on perceived intensity rather than specific heart rate. You should be able to hold a conversation when exercising during pregnancy. This is known as the “talk test.” Essentially, if you can chat but not belt out a song, you’re in the right zone.
| Member Tip: Integrate Oura with The Sculpt Society, a feel-good fitness platform that includes a comprehensive prenatal program with over 250+ classes, including prenatal strength, sculpt, yoga, post-partum recovery, plus pelvic floor & core support. All TSS x Oura Members receive daily workout suggestions aligned with your Oura Readiness Score, so you can move intentionally, recover fully, and stay consistent. Receive 50% off your first two months of The Sculpt Society app by using the code OURA at checkout. |
The Best Exercises to Do During Pregnancy
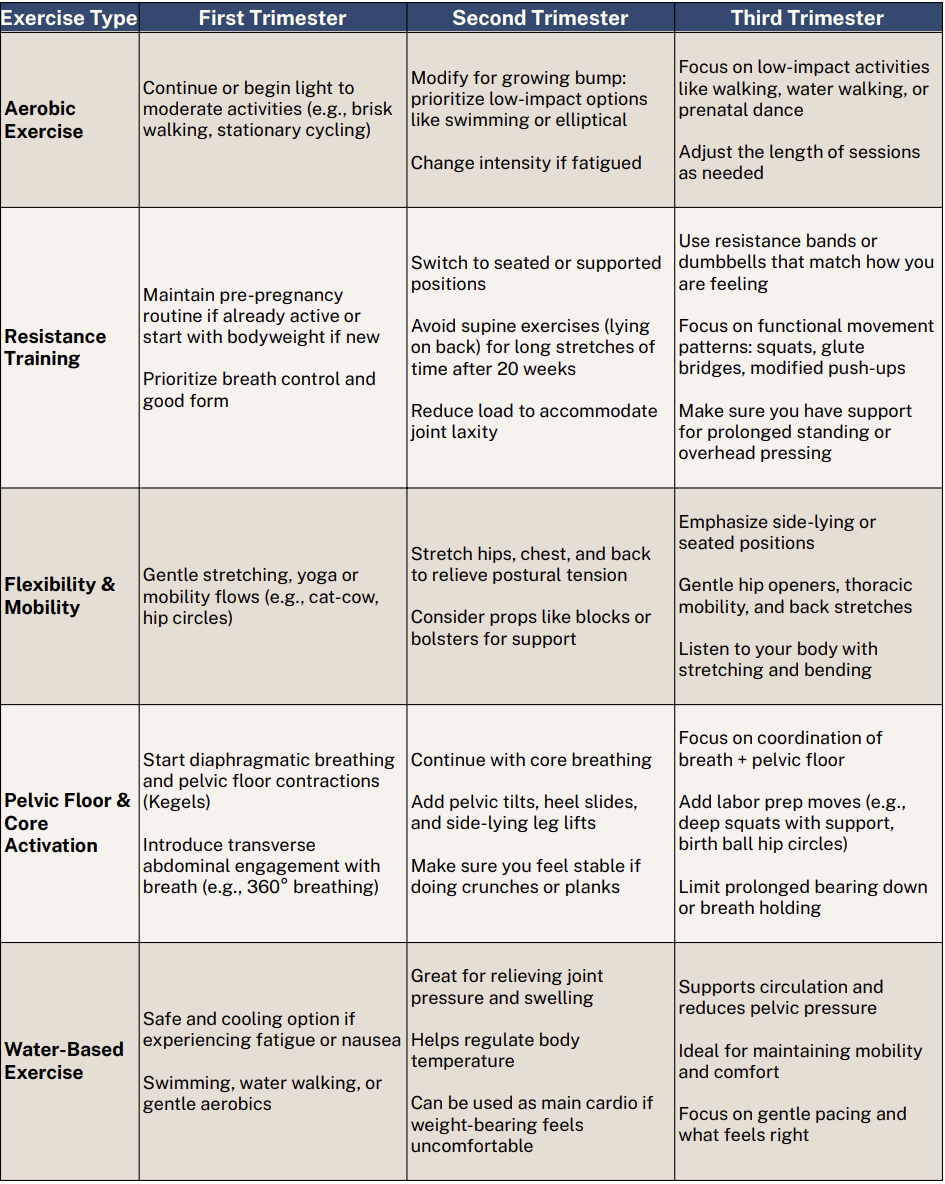
While there’s no single best workout while pregnant, the “best” approach is a balanced one. This means a trimester-specific blend of aerobic, resistance, mobility, and pelvic floor exercises that adapts to your body’s changing needs.
Below are key elements in a fitness routine that can support your health, your baby’s development, and postpartum recovery.
- Aerobic Exercise: Continuous rhythmic activity that raises your heart rate and has you breaking a sweat, such as brisk walking, swimming, cycling, or dancing. Supports cardiovascular health, placental blood flow, and glucose metabolism.
- Resistance Training: Strength-based exercises using bodyweight, resistance bands, or light weights to maintain muscle mass, joint stability, and posture.
- Flexibility & Mobility Work: Stretching, yoga, and joint mobility movements to reduce tension, improve posture, and accommodate your changing body.
- Pelvic Floor & Core Activation: Focused work on deep core muscles (transverse abdominis) and pelvic floor (levator ani group) to support intra-abdominal pressure, bladder control, and labor preparation.
- Water-Based Exercise: Low-impact aquatic activities like swimming or water aerobics that reduce joint strain and help with swelling and circulation.
READ MORE: What Happens to Your Body During Pregnancy, According to Oura Member Data
How to Adjust Prenatal Exercise by Trimester
LEARN MORE: How These Women Are Using Oura as a Guide During Pregnancy & Motherhood
Exercises to Avoid During Pregnancy
Most movements are safe with modification—but some should be adjusted or skipped altogether, especially as your pregnancy progresses. If an exercise puts you at risk of losing your balance, falling, or getting hit in the abdomen, it is probably not a good exercise for pregnancy.
| Exercises to Limit or Avoid | How to Modify |
| Prolonged supine exercises (lying on your back) after 20 weeks | Perform movements in side-lying, seated, or inclined positions instead, or break up time lying on your back with other movements |
| High-impact or contact sports | Switch to low-impact activities like swimming, walking, or indoor cycling |
| Workouts in hot or humid environments (risk of overheating) | Exercise in a temperature-controlled space, stay well hydrated, wear breathable clothing, and pause if you feel too hot |
| Heavy lifting with poor mechanics | Use lighter weights with controlled form; consider weight machines instead of free weights, prioritize proper posture and breathing |
| Prolonged breath-holding under strain (Valsalva maneuver) | Exhale during exertion and keep breathing continuously throughout movement |
| Crunches or intense core exercises | Focus on deep core engagement, pelvic tilts, bird-dogs, and modified side planks |
| Exercises with high fall or abdominal injury risk (e.g., skiing, horseback riding, boxing) | Pause these exercises until postpartum, and exchange them for stable, predictable movements with low balance demands like walking or water workouts |
7 Common Prenatal Fitness Myths, Debunked

You shouldn’t exercise if you didn’t before pregnancy.
False! The truth is that for most healthy pregnancies, it’s safe and encouraged to start a moderate exercise program, like walking or prenatal yoga, even if this is brand new for you. Always consult your doctor first.
Keep your heart rate below 140 bpm.
False! This is an outdated guideline. Focus on the “talk test”—you should be able to carry on a conversation while exercising. Your resting and exercise heart rates naturally increase during pregnancy, so focusing on those alone is less helpful.
Don’t lift weights or lift anything “heavy.”
False! Strength training is highly beneficial during pregnancy and may reduce risks like preeclampsia and gestational diabetes. Focus on proper form, controlled movements, and listen to your body. You’ll be lifting a baby soon enough!
Avoid all abdominal exercises.
False! While traditional crunches may not feel comfortable, safe and effective core exercises (like pelvic tilts and modified planks) are crucial for supporting your growing belly, improving posture, and aiding postpartum recovery.
Exercise increases the risk of miscarriage or preterm labor.
False! For healthy, uncomplicated pregnancies, moderate exercise does not increase the risk of miscarriage or preterm labor. In fact, it can reduce the risk of complications.
You shouldn’t exercise on your back after the first trimester.
False! Prolonged lying flat on your back can compress a major blood vessel (vena cava) because the growing uterus puts pressure on it. For most people, some short periods of exercise while lying on your back are generally acceptable unless you feel dizzy or nauseous. Prop up your right side (right side higher) with a wedge if needed.
Running is off-limits during pregnancy.
False! If you were a runner before pregnancy and have an uncomplicated pregnancy, you can usually continue running at a moderate, comfortable pace. It may not be the time for everyone’s personal bests, but maintaining activity is good.
RELATED: Pregnancy Symptoms by Trimester: What’s Normal—and What Might Be a Red Flag












