Not sleeping well? You’re not alone. The CDC estimates about 70 million Americans have a chronic sleep problem, such as sleep apnea or insomnia. Yet research suggests that more than 40 million people don’t get a proper diagnosis or treatment.
Those who do receive a diagnosis have often undergone an intensive sleep study, known as polysomnography, or PSG. These studies are usually performed in a clinical setting as they require an elaborate setup with medical-grade equipment, plus a trained technician to read the results.
Curious to learn more about what’s involved in a PSG study? Keep reading to find out. Plus, learn how it compares to a wearable sleep tracker like the Oura Ring, which is more comfortable and less invasive, while providing research-validated sleep data over a longer period of time.
A Brief History of Sleep Tracking
“Up until roughly the 1950s, people thought that sleep was just a passive on/off switch,” explains Raphael Vallat, PhD, neuroscientist, sleep researcher, and senior machine learning data scientist at Oura. “This view changed with the development of electroencephalography (EEG), a method to measure electrical brain activity, or brain waves.”
As it turns out, there’s a lot happening in your brain while you sleep. Using EEG, scientists in the ‘50s discovered that sleep is in fact composed of four different sleep stages (N1, N2, N3, and REM), each of which has a different pattern of brain waves. You may have heard of these stages referred to by their more colloquial terms — light (which comprises N1 and N2), deep (aka N3), and REM.
To this day, the sleep stages are still defined and scored through looking at the brain waves, together with muscle activity and eye movements. This is referred to as polysomnography, or PSG. PSG is the gold-standard to measure sleep stages or diagnose sleep disorders.
READ MORE: What Are the Stages of Sleep?
Who Should Have a PSG Sleep Study?
If you suspect you are not sleeping well, your doctor may refer you to have a PSG sleep study, which can be used to diagnose sleep disorders. A PSG sleep study tests for disorders such as sleep apnea, insomnia, periodic limb movement disorder, narcolepsy, or REM sleep behavior disorder.
Patients usually have to undergo the PSG study in a clinical sleep center or hospital setting, but on some occasions it can be performed at home. Most sleep studies occur over only one night, capturing a snapshot of your sleep at a moment in time.
READ MORE: Sleep Apnea, Defined — And How to Treat It
What Happens During in a PSG Sleep Study?
PSG is the gold-standard to measure sleep stages and requires an intensive setup with a lot of medical-grade equipment. While you sleep, the PSG records:
- Brain waves (electroencephalography, EEG)
- Heart rate (electrocardiogram, ECG)
- Eye movements (electrooculography, EOG)
- Muscle & leg movements (electromyography, EMG)
- Blood oxygen level (peripheral oxygen saturation, SpO2)
- Respiratory rate
Each of these measurements requires an extensive setup of wires positioned in a precise location on your head (EEG), your chest/abdomen (ECG), face (EOG), chin and legs (EMG), and finger (SpO2). A trained technician will place electrodes connected to wires in each location and confirm that signals are being recorded prior to lights off. This process can take 60 minutes to two hours before bedtime.
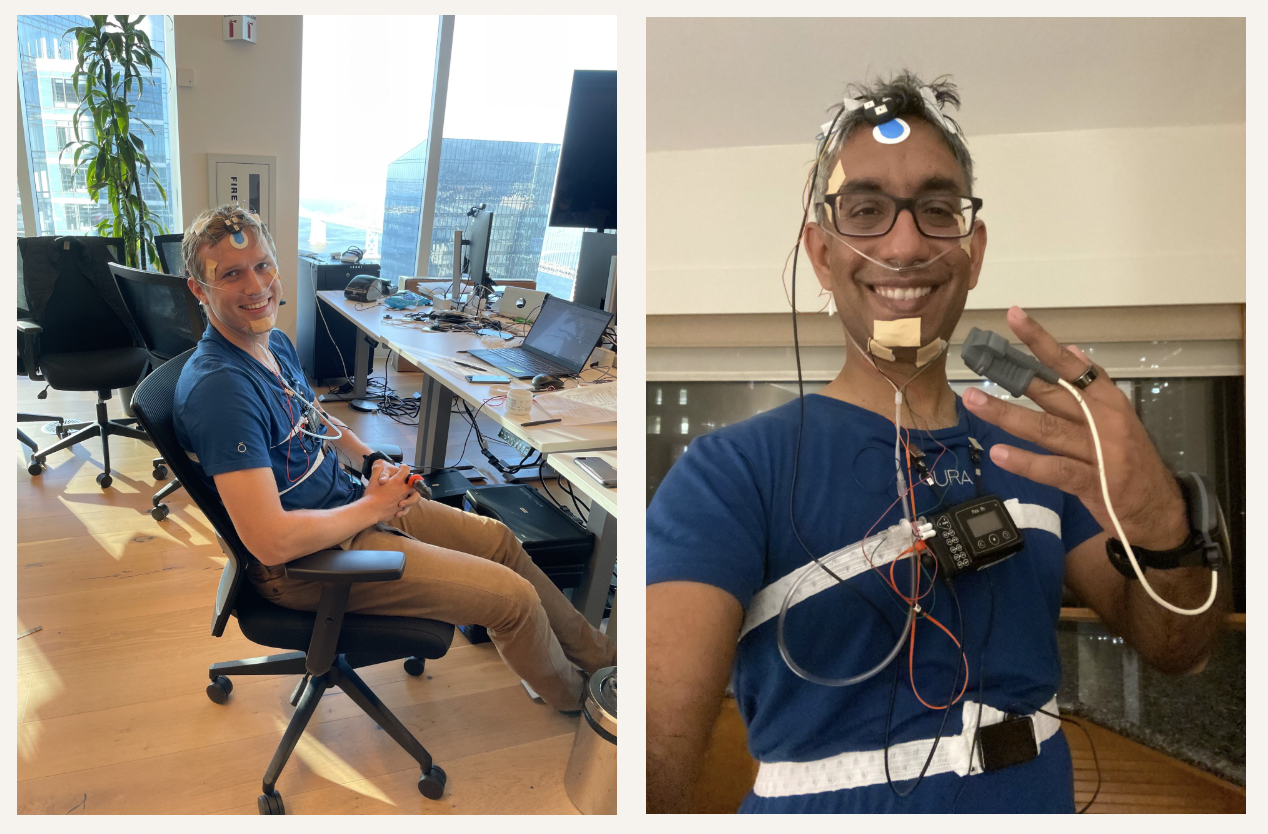 Oura’s research data engineer Jurre Wouters and Head of Science Shyamal Patel, PhD, prepare to track a night of sleep wearing a standard PSG setup.
Oura’s research data engineer Jurre Wouters and Head of Science Shyamal Patel, PhD, prepare to track a night of sleep wearing a standard PSG setup.
As one might imagine, a patient may experience some discomfort with all these cumbersome wires and devices hooked up while trying to sleep, Vallat says. “Plus, trying to sleep in a new environment that is not familiar can be even more difficult, and may in fact lead to an outcome of poorer-than-usual sleep quality.”
What Do a PSG Sleep Study Results Mean?
In the morning, after the completion of the sleep study, your sleep data is analyzed by a highly trained technician, known as a Registered Polysomnographic Technologist, or RPSGT.
The RPSGT will evaluate several aspects of your sleep, including:
-
- Sleep onset latency: how long it takes to fall asleep
- Sleep efficiency: how much time is spent asleep over the time in bed
- Time spent in each of the five sleep stages: N1, N2, N3, REM plus awake time
- Apnea severity
- Heart rate during sleep
To determine your sleep stages throughout the night, the technician will first divide your PSG data into 30 second increments, called epochs. Then, they will evaluate each epoch based on the well-defined guidelines set out by the standard scoring manual to determine in which stage of sleep each epoch is categorized.
For example, during deep sleep (or N3 sleep), very large-amplitude slow waves (roughly one per second) can be seen on the EEG. During rapid eye movement (REM) sleep, the brain electrical activity is almost indiscernible from wakefulness, but the body is completely paralyzed and the eyes are moving very quickly — hence the name REM.
After the data is classified, a sleep doctor will review the results and determine possible paths to improve your sleep, such as working on sleep health, reducing stress, or other lifestyle changes. If a sleep disorder such as sleep apnea has been detected, your doctor may recommend an intervention such as a CPAP machine.
RELATED: Why You Shouldn’t Stress About Getting the “Perfect” Night of Sleep
What Are the Drawbacks of a PSG Sleep Study?
Sleep quality: Because of the intensive PSG setup and the fact that patients have to sleep in a clinical setting, the night of sleep that a PSG study analyzes can be far different from a more natural night of sleep at home.
Data analysis limitations: Determining sleep staging is a difficult and time-intensive process that can take up to 2 hours by a well-trained technician. Since the stages are determined by a person, some variation occurs in terms of agreement of raters, particularly in transitional periods (going from one stage of sleep to another). In fact, agreement among multiple technicians scoring the same night is usually about 83%, according to this 2013 study.
Moreover, the same technician scoring the same night on separate occasions may only agree with themselves for about 90% of the night. “In other words, different human experts presented with the same recording will likely end up with somewhat dissimilar sleep stages, and even the same expert presented with the same recording assessed at two different time points will arrive at differing results,” as Vallat noted in this 2021 paper, co-authored by Prof. Matthew Walker.
Cost: The cost of a PSG sleep study can range from $600 to $5,000. What you will spend depends on many factors, such as the clinic or center where the test is performed, what company or hospital runs it, and what your health insurance will pay. Contact your health insurance provider to find out what they will cover for a sleep study.
Oura Ring: An Alternative to PSG Sleep Studies
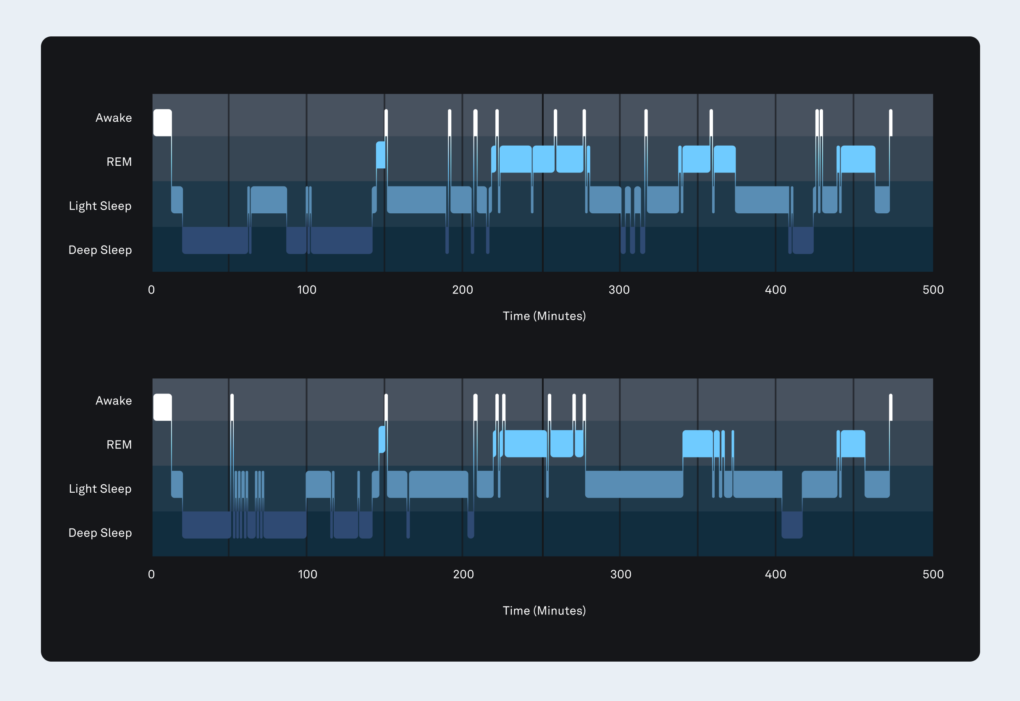
The top graph shows the sleep stages across the night determined with gold standard polysomnography. The bottom graph shows the sleep stages predicted by the Oura Ring algorithm (accuracy = 84%).
Not everyone needs (or wants) a sleep study performed in a sleep lab. That’s why many people choose a sleep wearable such as Oura Ring, which provides a more comfortable—and still highly accurate—way to track your sleep data. To name a few of the advantages that Oura Ring offers:
- It’s comfortable. With Oura Ring, you won’t have to wear a bunch of wires or headsets to bed to track your sleep; all you need to do is slip a lightweight ring on your finger.
- It’s less costly. Oura Ring starts at $299. The first month of membership is on us, and $5.99/mo afterwards.
- It tracks your sleep over the long term, not just one night. Because you can wear Oura Ring every night over a long period of time, you can see trends and correlations in your sleep data, which can help you learn which behaviors and habits help you sleep your best.
- It doesn’t require a doctor’s referral, nor do you have to spend a night in a clinic or hospital.
- It’s highly accurate. While using an Oura Ring is not the same as a PSG (as it does not measure electrical brain activity or eye movements), research shows that Oura’s latest sleep staging algorithm achieves 79% agreement with gold-standard polysomnography (PSG) for 4-stage sleep classification. By contrast, most commercial wrist-based wearables are limited to 60-65% agreement.
- It does so much more than just track your sleep. Oura Ring measures several parameters that are also changing extensively during the different sleep stages, such as heart rate, HRV, temperature trends, and movement.
LEARN MORE: How Does the Oura Ring Track My Sleep?
About the Oura Expert
Raphael Vallat, PhD, is a senior machine learning data scientist at Oura. He previously worked as a sleep researcher in the Center for Human Sleep Science at University of California Berkeley (Prof. Matt Walker‘s lab). He has published extensively on the topic of sleep and human health, and his work has been featured in several major news media and podcasts. In his free time, you can find him enjoying precious moments with his amazing wife and daughter, playing music, or hiking with friends.




