- Trouble sleeping during menopause? You’re far from alone. Research shows that sleep disturbances are prevalent among women going through perimenopause and menopause.
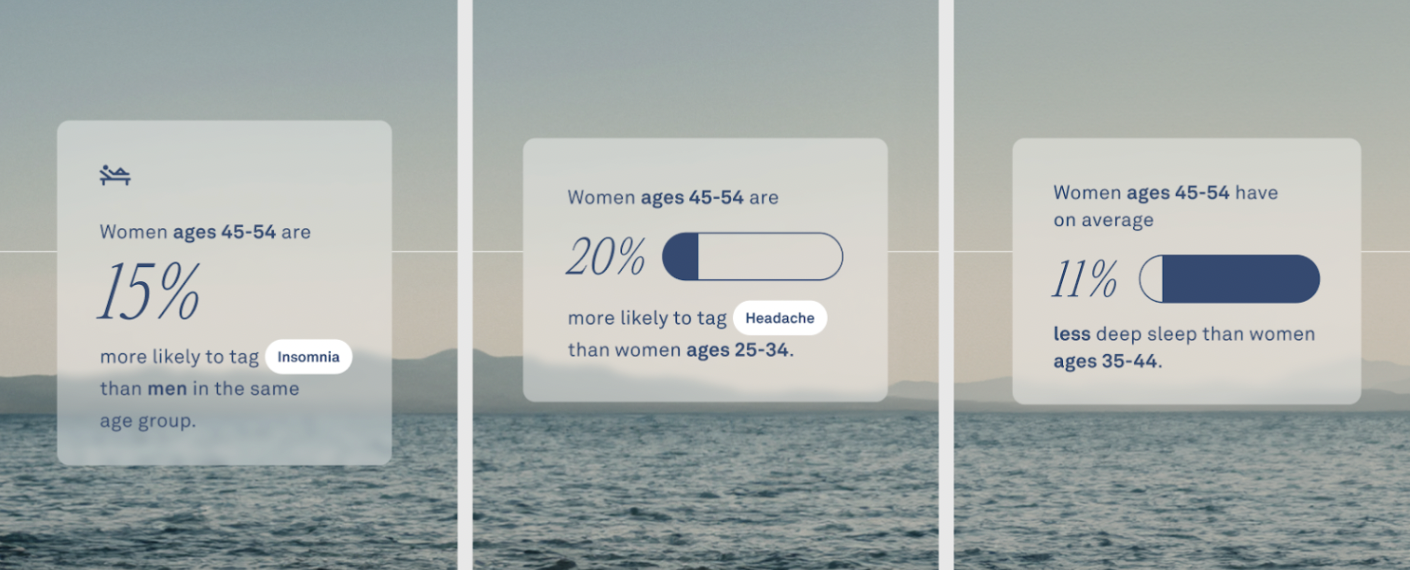
- This is supported by aggregate Oura data, which shows that female members aged 45 to 54 are 15% more likely to tag “insomnia,” compared to men in the same group. They also get about 11% fewer minutes of deep sleep than women aged 35 to 44.
- To address sleep disturbances during menopause, you can consider some science-backed solutions such as making dietary changes, practicing good sleep hygiene, considering hormonal therapy, and more.
Menopause, which typically begins around age 50, marks the end of a woman’s reproductive years. While there are many changes that come with this life stage, many menopausal women suddenly find they’re having trouble sleeping.
If this is a familiar frustration, know you’re not alone. Research suggests that up to 47% of women experience sleep disturbances during perimenopause, while up to 60% do so in menopause. And Oura data backs this up, which we’ll explore later on.
Another small study found that menopausal women experience more frequent awakenings, get less total sleep, have lower levels of melatonin, delayed sleep onset latency, have less deep sleep, and reduced next-day alertness levels.
The reasons for all these sleep troubles during menopause vary, but are largely tied to hormonal fluctuations, physical symptoms, and psychological factors, among others — more on this below.
Rest assured: There are strategies you can use to sleep better during menopause, empowering you to navigate this transition successfully — and restfully.
What is Menopause?
Menopause marks the end of a woman’s reproductive years, and typically occurs between the ages of 45 and 55. Menopause is defined as the cessation of menstruation for 12 consecutive months, and is marked by a decline in estrogen and progesterone levels.
What is Perimenopause?
Perimenopause is the transitional phase that leads up to menopause, characterized by hormonal fluctuations and irregular menstrual cycles. While perimenopause can begin as early as your 30s, it typically begins in your 40s.
How Your Hormones Shift During Menopause
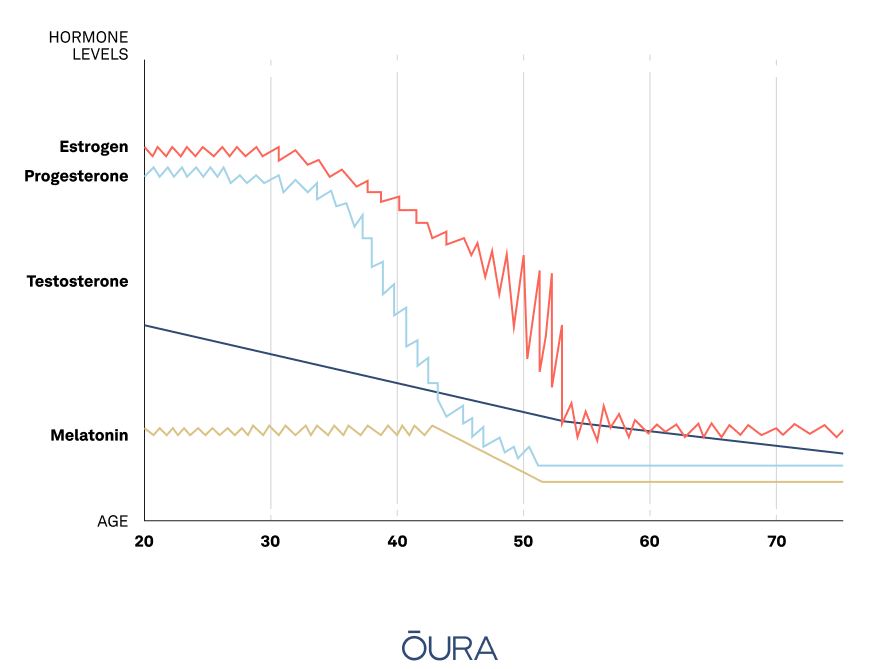
The main hormones involved in the menopause stage are estrogen and progesterone, the female sex hormones. These regulate a wide range of bodily functions, including the menstrual cycle, bone density, and brain function. When you enter menopause, the levels of these hormones lower, which can have significant consequences for your health, well-being, and sleep.
In addition, during menopause melatonin, the sleep hormone, decreases; cortisol, the stress hormone, increases; and testosterone levels lower to about one-quarter of what they were at their peak. Testosterone is commonly associated with male physiology, but it also plays a vital role in women’s health. In women, testosterone contributes to muscle strength, bone density, libido, and overall sense of well-being.
Common Menopausal Symptoms
This rollercoaster ride that your hormones take during menopause can lead to many unwanted symptoms during menopause — a combo of which add up to poor sleep.
For starters, as estrogen and progesterone levels decline, it may disrupt your circadian rhythm, or internal clock. This can make it harder to fall asleep and stay asleep throughout the night.
These hormonal changes can also contribute to night sweats and hot flashes, which can further disrupt sleep by causing discomfort and night-time awakenings.
Moreover, psychological factors associated with menopause, such as elevated stress and anxiety, mood swings, and depression, can exacerbate sleep problems. If you find yourself in a state of emotional arousal at night, it’s often difficult to get a solid night’s sleep.
READ MORE: Try Oura’s Guided Sleep Meditations for Deep and Restful Sleep
What Oura Data Says About Menopause and Sleep
According to aggregate and anonymous Oura member data, women members aged 45 to 54 are 15% more likely to tag “insomnia,” compared to men in the same group. This age group also gets about 11% less deep sleep than women aged 25 to 34.
Additionally, women in that age group are more likely to use the following tags, listed below in order of frequency:
- Migraine
- Hot flashes
- Night sweats
- Headache
Sleep Disturbances During Menopause
Below, dive deeper into why these sleep disturbances typically occur during menopause.
Insomnia During Menopause
Menopausal women commonly experience insomnia, characterized by difficulty falling asleep or staying asleep. In fact, a 2020 study reported it as one of the most commonly reported symptoms of menopause.
Fluctuating hormone levels have a direct impact on sleep quality. For instance, lower progesterone levels can make you feel more awake at night, and lower melatonin levels can make sleep more of a challenge.
Typically, melatonin naturally increases in the evening in line with sleep onset, to help you feel tired when the sun goes down. If melatonin levels are disrupted, you may struggle to fall asleep and stay asleep.
Finally, mental health issues can also play a role in insomnia: Several studies have found a link between depression, anxiety, and a higher likelihood of insomnia in menopausal women.
Snoring During Menopause
If you notice yourself snoring more frequently during this phase, know that it’s normal. However, it can impact your overall sleep quality. As estrogen levels decline during menopause, muscle tone in the upper airway, including the tongue, soft palate, and throat muscles, decreases. This can lead to increased airway resistance, making breathing more difficult during sleep and increasing the likelihood of snoring and sleep apnea.
Note that snoring is common and in most cases, harmless. But if your snoring wakes you up at night or you feel noticeably more tired in the morning, it could be a sign of sleep apnea.
READ MORE: Does Mouth Taping Really Help With Snoring?
Sleep Apnea During Menopause
Sleep apnea is a sleep disorder that occurs when breathing stops and starts repeatedly during sleep, and menopausal women seem to be at an increased risk of developing it. One study found that up to 67% of postmenopausal women have obstructive sleep apnea.
In addition to the loss of muscle tone in the upper airway, menopausal women may also experience weight gain or changes in body fat distribution, which can contribute to sleep apnea. Excess weight around the neck and throat area can narrow the airway and make it more difficult to breathe during sleep.
Other warning signs of sleep apnea include dry mouth, morning headaches, or gasping for air.
READ MORE: The Surprising Link Between Menopause and Sleep Apnea
Restless Legs Syndrome During Menopause
Restless legs syndrome (RLS) affects individuals with an uncontrollable urge to move their legs, especially between 10pm and 4am.
This neurological disorder is thought to exacerbate during menopause due to fluctuating estrogen levels impacting central nervous system chemicals like dopamine and glutamate. However, researchers still need to conduct further studies to pinpoint the precise mechanism.
8 Strategies to Sleep Better During Menopause

Difficulty sleeping during menopause doesn’t mean you’re relegated to sleep badly for the rest of your life. Improving your sleep is within your control, thanks to a number of science-backed solutions, including lifestyle changes, dietary habits, environmental factors, and more.
In fact, a meta-analysis of 16 randomized controlled trials with more than 2,000 perimenopausal and menopausal women found that behavioral interventions like exercise, mindfulness, and relaxation had a significant effect on improving sleep quality.
1. Improve Your Overall Sleep Hygiene
Sleep hygiene refers to your habits and environment that prep you for a good night’s sleep. Start with these tried-and-true strategies below to ensure proper sleep hygiene during menopause (though they’re also important during any stage of life!).
- Keep a regular sleep-wake schedule
- Lower the temperature in your bedroom (this especially helps to combat night sweats and hot flashes)
- Avoid screens and blue light exposure at least one hour before bed
- Use a white noise machine to block out distracting noises in the environment
- Avoid eating within two hours before bedtime
READ MORE: How to Improve Your Sleep Hygiene
2. Relax Intentionally Before Bed
Studies show that relaxation practices like mindfulness, meditation, breathing, or reading improve sleep quality. These habits help you mentally unwind, helping to alleviate stress and get you ready for bed.
| Member Tip: You can access a range of guided meditations and breathing exercises directly in the Oura App’s Explore content. |
3. Maintain A Healthy Weight
Despite the challenges of weight management during menopause, there are abundant strategies to proactively maintain a healthy weight — strategies that offer additional benefits like better mental health and sleep!
Embracing a balanced lifestyle with regular exercise and nutritious eating habits not only reduces the risk of sleep apnea and snoring but also has the potential to alleviate bothersome menopausal symptoms such as hot flashes.
4. Adjust Your Diet
Studies suggest that it’s a good idea to avoid spicy foods, hot drinks, caffeine, sugar-sweetened beverages, and sugary or processed foods close to bedtime, if possible.
These foods and drinks increase your body temperature and nighttime heart rate, potentially triggering hot flashes and night sweats, making it difficult to fall asleep, and leading to more frequent awakenings.
Consider eating lighter meals in the evening and have more foods rich in soy like tofu and soy milk. Soy contains isoflavones, plant compounds that mimic estrogen in the body and have been associated with fewer menopausal symptoms. In fact, one study found that 30 mg of soy isoflavones reduces hot flashes by up to 50%.
READ MORE: 8 Foods and Drinks For Better Sleep (And 4 To Avoid!)
5. Avoid Alcohol and Sedatives
Alcohol worsens menopause symptoms, triggering symptoms like hot flashes and night sweats. What’s more, alcohol and other sedatives have a relaxing effect on the muscles of the body, including those in the upper airway. When these muscles relax, they can cause the airway to narrow, making it more difficult to breathe during sleep. This can worsen snoring and sleep apnea. In fact, higher levels of alcohol consumption have been shown to increase the risk of sleep apnea by 25%.
An additional downside: Alcohol also depletes dopamine, which will make your fluctuating mood sharply dip, leaving you feeling lower than ever. This has a direct impact on your sleep quality.
If you don’t want to forgo your favorite nightcap, consider switching to a non-alcoholic version. The ritual of drinking a yummy beverage before bed may still help you unwind — without the downsides of alcohol!
READ MORE: 7 Tasty Alcohol-Free Drink Ideas for Dry January
6. Sleep On Your Side for Sleep Apnea
Thanks to gravity’s effects on the body, sleeping on your back can cause the tongue and soft palate to collapse to the back of your throat, blocking your airway, leading to snoring, and increasing the duration and frequency of sleep apnea.
Research has even shown that left-side sleeping reduces the severity of sleep apnea.
RELATED: What’s the Best Sleeping Position for Breathing Problems?
7. Choose Breathable Bedding and Pajamas
Opt for lightweight, breathable pajama fabrics such as cotton or linen to help regulate body temperature during the night. This can help alleviate night sweats and hot flashes. Additionally, choose bedding that allows for better air circulation — consider having multiple layers of bedding so you can easily adjust to your comfort level in the night.
8. Take an Evening Stroll
An evening stroll has numerous benefits that directly impact sleep: exercise releases endorphins to alleviate stress and help you unwind before bed, helps you digest your dinner, it reduces symptoms of restless leg syndrome and joint pain, and improves your metabolic health to reduce the risk of sleep apnea.
One study found that middle-aged women slept better and for longer on days that they walked more.
Hormone Replacement Therapy (HRT) and Sleep
If you’re experiencing severe menopause symptoms, such as persistent hot flashes, insomnia, extreme night sweats, or significant mood changes, you might want to consider hormone replacement therapy (HRT). Only about 14% of women currently use HRT, but it’s been proven to enhance sleep quality during menopause. For instance, one study found that HRT can reduce the severity of sleep apnea by as much as 75%.
Seek support from your healthcare provider if you are experiencing menopause symptoms that significantly disrupt your daily life and quality of sleep.

HRT involves administering estrogen and/or progesterone to alleviate menopausal symptoms. Research has shown that estrogen therapy can increase total sleep time, reduce the frequency and severity of hot flashes, and improve overall sleep efficiency in menopausal women.
Progesterone, another hormone commonly used in HRT, may also have a beneficial effect on sleep by promoting relaxation and reducing anxiety.
However, it’s essential to weigh the potential benefits of HRT against its possible risks and side effects. HRT carries an increased risk of certain health conditions, including breast cancer, blood clots, and stroke. So if you are considering it, it’s crucial to discuss your individual risk factors and preferences with your healthcare provider.
Above all, if you’re concerned and frustrated with poor sleep during menopause, know that you don’t have to suffer in silence. Seeking support from a professional can help you feel empowered in this new phase of your life.
READ MORE: 9 Science-Backed Herbs and Supplements for Better Sleep











