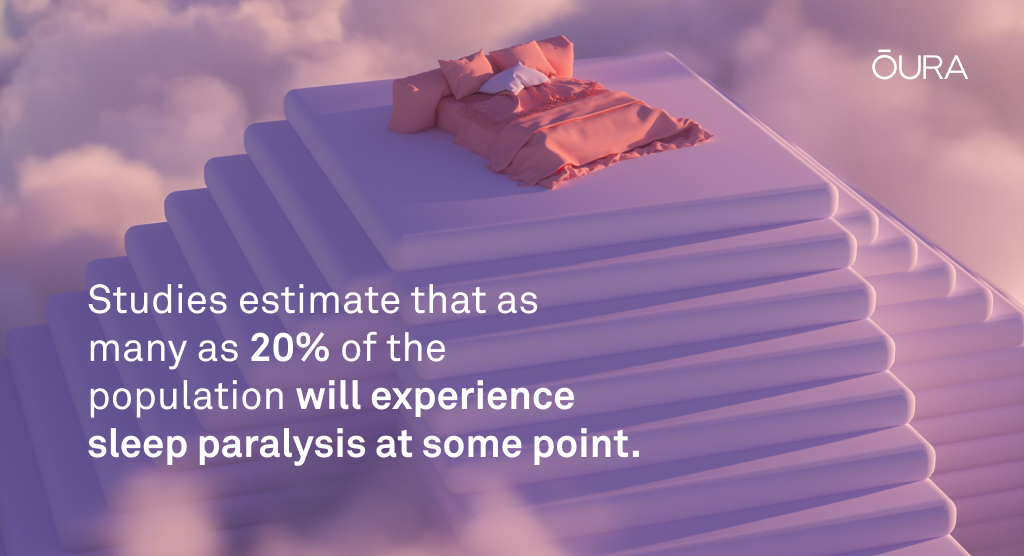
- Sleep paralysis, a sleep condition that can be alarming (but is not harmful) affects about 20% of the population.
- Characterized by muscle immobility and speechlessness, this condition can be triggered by stress and underlying sleep disorders.
- Oura helps you get a clearer idea of what happens to your body as you sleep.
What Is Sleep Paralysis?
Sleep paralysis is a complex phenomenon that involves various factors, including sleep hygiene, stress levels, and underlying sleep disorders. While estimates vary, research suggests that about 20% of the population will experience sleep paralysis at some point.
Sleep paralysis is characterized by temporary muscle immobility and speechlessness during the transition from wakefulness to sleep. The loss of muscle control is known as muscle atonia and it’s typically accompanied by vivid hallucinations. While these hallucinations may seem otherworldly at times, there’s nothing supernatural about it.
Sleep paralysis is a well-documented sleep disorder with scientific explanations rooted in neurobiology and sleep physiology. Researchers believe it’s caused by irregularities in REM sleep, particularly when you regain awareness while entering or coming out of REM.
Another common side effect of sleep paralysis is the sensation of chest pressure, often leading to gasping for breath upon awakening. These disturbances can disrupt your normal sleep cycle, causing fragmented sleep patterns and reduced sleep quality.
Certain health conditions can also increase your likelihood of experiencing sleep paralysis. These conditions include obstructive sleep apnea, insomnia, excessive daytime sleepiness, and disturbances in your circadian rhythm.
READ MORE: Sleep Apnea, Defined – And How To Treat It
Oura and Sleep Paralysis
While Oura Ring can’t diagnose or treat sleep paralysis, the insights your Oura App provides can help you improve your sleep quality. Oura’s unique ability to combine heart rate, movement, temperature, and heart rate variability (HRV) into its sleep staging algorithm helps you get a clearer idea of what happens to your body as you sleep. Plus, your Sleep Score will tell you how well you sleep every night, all based on personalized, real-time data points.
In addition, gaining a better understanding of the disorder itself is vital. Below, we debunk seven common myths and misconceptions surrounding sleep paralysis.
READ MORE: How Does the Oura Ring Track My Sleep?
6 Common Misconceptions About Sleep Paralysis
Misconception #1: Sleep paralysis is harmful to your health.
Sleep paralysis is generally regarded as harmless, and you are likely to encounter it only once or twice in your life. However, it can serve as a symptom of an underlying sleep disorder.
For instance, recurrent episodes of sleep paralysis can be a sign of narcolepsy, a sleep disorder characterized by unstable boundaries between wakefulness and sleep.
Another major concern with sleep paralysis is its emotional and psychological impact. The vivid hallucinations, the sensations of pressure, and the overwhelming sense of being unable to escape can contribute to feelings of stress, anxiety, and depression.
Oura member Dada J. has found the app useful for managing stress. She has this to say about her experience, “I do red light therapy while meditating and using the Unguided Sessions feature in the Oura App. This combination has been incredibly helpful in achieving a deeper level of relaxation. Plus, the ability to track my heart rate variability (HRV) and breathing rate during meditation sessions has been incredibly helpful.”
Misconception #2: Sleep paralysis is a sign of a mental health disorder.
While sleep paralysis is more common in individuals with mental health disorders (34.6% of psychiatric patients with anxiety disorders reported lifetime sleep paralysis), it’s not a sign of mental health disorder.
Some factors that have been found to cause sleep paralysis include:
- Prescription medications: Certain medications that affect neurotransmitters in the brain, such as antipsychotics and antidepressants, may alter the balance of chemicals involved in sleep regulation and cause sleep paralysis episodes.
- Stress and anxiety: Emotional factors, such as high-stress levels or sleep-related anxiety, can trigger or exacerbate sleep paralysis. Stressful life events and traumatic experiences can also contribute to the disorder.
Misconception #3: Sleep paralysis only happens to people with sleep disorders.
Although sleep paralysis is more commonly seen in people with sleep disorders like narcolepsy or sleep apnea, it can happen to anyone of any age.
However, it tends to be more noticeable in specific groups, particularly young adults. The exact reasons for this are not entirely understood, but it is believed to be associated with hormonal fluctuations, changes in sleep patterns, and lifestyle factors.
Misconception #4: Sleep paralysis only occurs when you sleep on your back.
Sleep paralysis can happen regardless of your sleep position, as it is more closely linked to the quality of your sleep.
Nonetheless, sleeping on your back may increase your chances of experiencing sleep paralysis as it makes you more susceptible to being awakened by snoring or sleep apnea. On the other hand, sleeping on your side or stomach may potentially reduce the likelihood of sleep paralysis episodes, although it’s not guaranteed to prevent them.
If you tend to roll over and sleep on your back, putting a pillow behind your back can help keep you in a position that reduces your chances of experiencing sleep paralysis.
READ MORE: 8 Popular Sleeping Positions: Find Out What They Mean For Your Health
Misconception #5: You can’t breathe during sleep paralysis.
While sleep paralysis can create a suffocating sensation, it’s important to remember that you remain fully conscious during these episodes, and your breathing remains unaffected.
During sleep paralysis, the body’s voluntary muscles, including those responsible for breathing, experience temporary immobilization. This serves as a protective mechanism, preventing physical reactions to dreams that could potentially lead to injury. However, while voluntary muscle movement is restricted, the autonomic nervous system maintains control over vital functions such as breathing and heart contraction and relaxation.
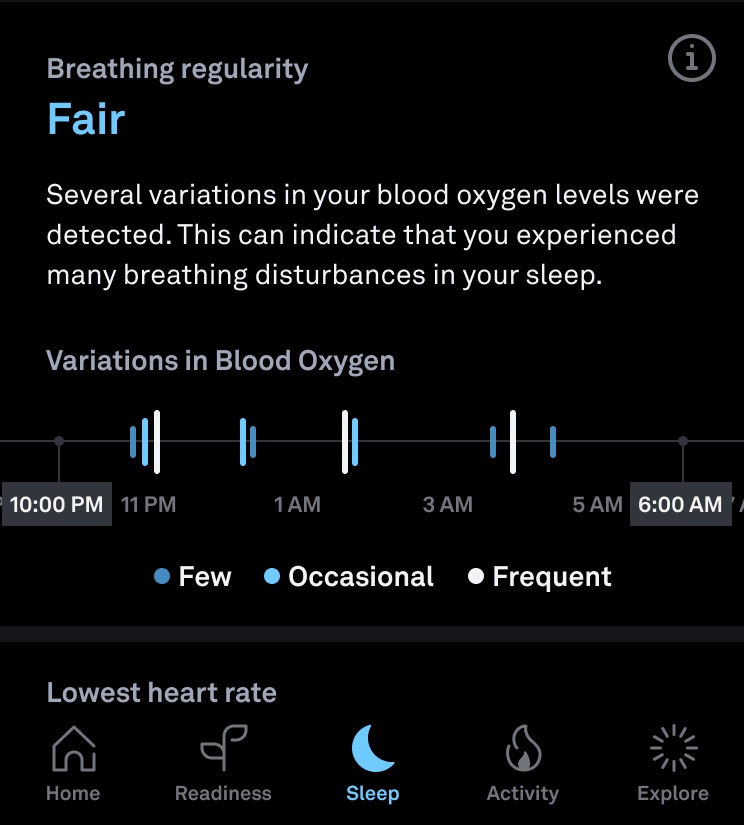
By checking the breathing regularity feature, Oura members can keep track of how many breathing disturbances they experience during the night. And, despite your mind telling you that you’re unable to breath, you can turn to this feature to rest assured that this is not the case.
RELATED: Understanding Your Respiratory Rate
Misconception #6: Sleep paralysis is always accompanied by hallucinations.
Not every episode of sleep paralysis will be accompanied by hallucinations, but these are common. According to research, the main reason you hallucinate during sleep paralysis episodes is because serotonin is released during REM. There are three main categories that these hallucinations fall into:
- Intruder hallucinations: These involve the perception of a dangerous person or presence in the room, usually a shadow figure that exudes menacing energy.
- Incubus hallucinations: Feelings of chest pressure and shortness of breath characterize these hallucinations. If figures are present, the pressure felt on the throat is due to them ‘restraining’ you while carrying out aggressive acts.
- Vestibular-motor (V-M) hallucinations (out-of-body experiences): V-M hallucinations can make you feel like you’re floating or having an out-out-body experience. This is when you see your own body from an external perspective and interpret it as if you have left your physical body.
It’s important to remember that as shocking as they are, hallucinations in this circumstance do not indicate mental illness or psychosis. They are a natural occurrence due to your brain being in partial wakefulness.
How to Prevent Sleep Paralysis Episodes
There is no cure for sleep paralysis, but adopting healthy sleep habits can contribute to better overall sleep, which helps reduce sleep paralysis. This includes limiting screen time before bed, avoiding caffeine and big meals before sleeping, winding down with meditation or reading, and maintaining a regular sleep schedule.
Oura’s Bedtime Guidance feature will assist you in determining the best time to go to bed. As bedtime approaches, you’ll also get suggestions on how to wind down for the night.
READ MORE: How to Improve Your Sleep Hygiene
When to Seek Professional Help
Unfortunately, in some cases, sleep paralysis can be very frequent and lead to a long-term lack of sleep. In this situation, you should seek professional help.
Health professionals can perform tests to try and find the root of your sleep paralysis. With this information, they can begin finding the best methods to lessen the severity of the disorder or stop it altogether. In some cases, they will prescribe certain sleep medicines.
Polysomnography (PSG) is a typical test conducted on people with sleep problems and involves monitoring and analyzing patients’ waking and sleeping patterns. Professionals may also recommend cognitive-behavioral therapy (CBT) as a therapeutic approach to treating the mental effects of sleep paralysis.
The effectiveness of these preventative measures will vary from person to person, so it’s a good idea to be patient as you try to find the best solution for you.