Oura is committed to creating tools that consumers and researchers can rely on. In light of this, we conducted an internal validation study, described in this blog, of the Oura Ring temperature sensor.
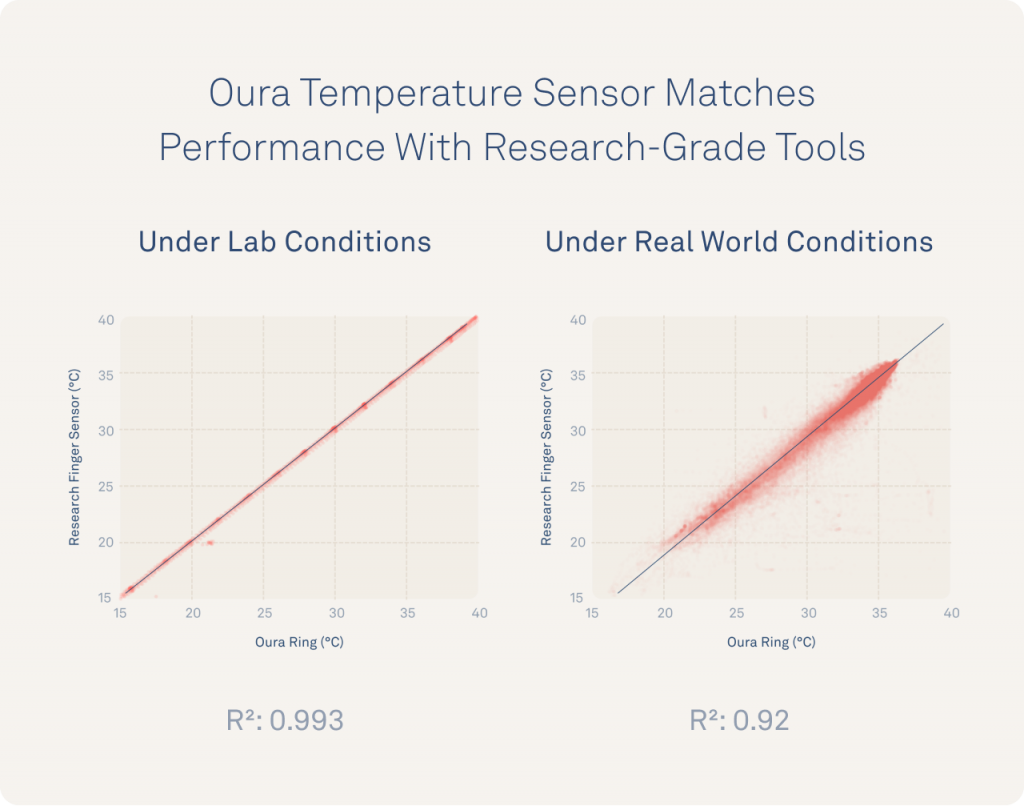
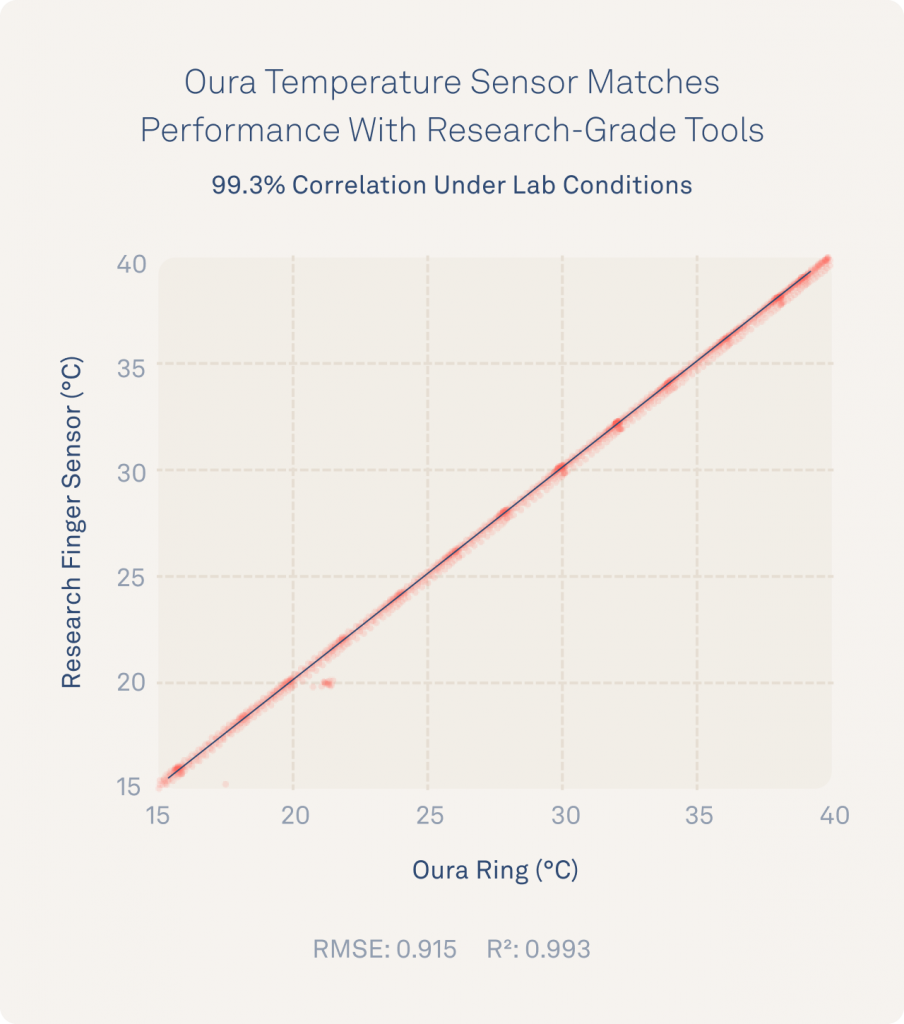
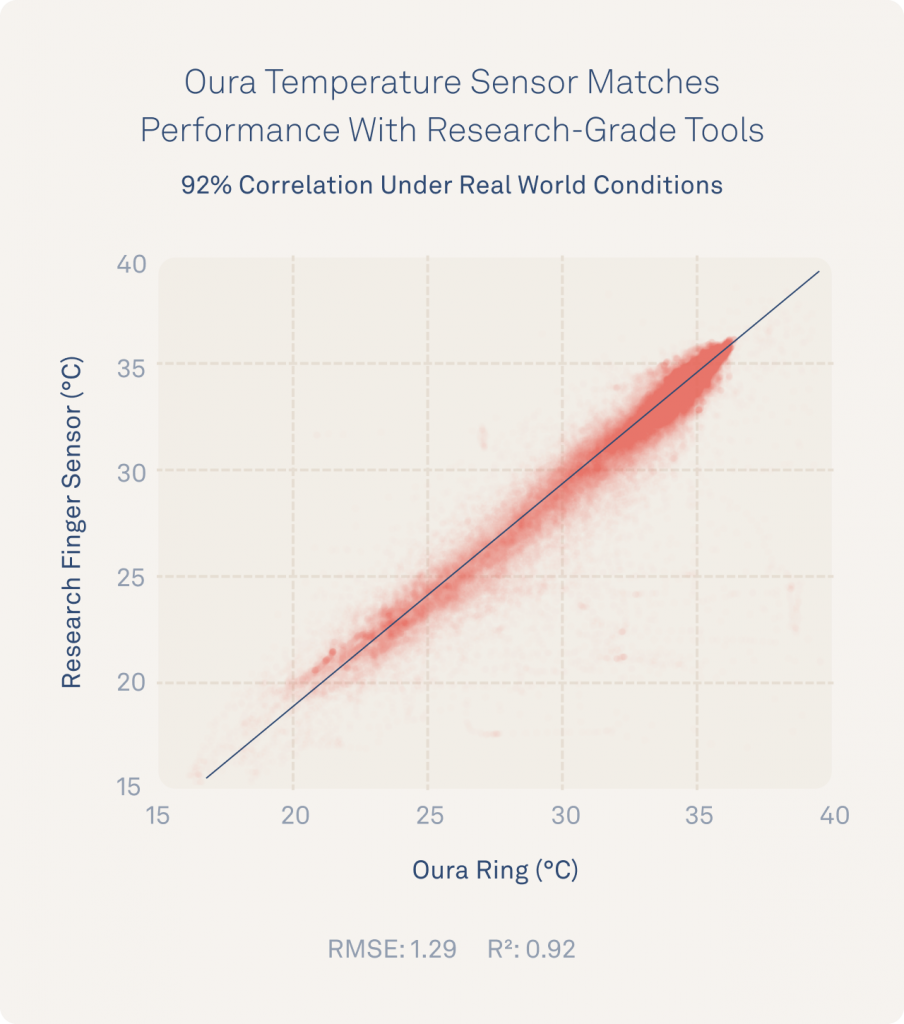
As a result of this study, Oura’s temperature sensor was validated to measure changes as precisely as 0.13°C (0.234°F), every minute. Oura’s performance matches near-perfect with the research-grade iButton at >99% under lab conditions, and 92% under real world conditions.
How Oura Measures Temperature
Oura measures your temperature every minute, directly from the underside of your finger. Access to this kind of temperature data provides a remarkably useful signal.
Although many people think of measuring temperature as a thermometer under your tongue, Oura is part of the growing scientific movement that is making major updates to how we interpret body temperature:
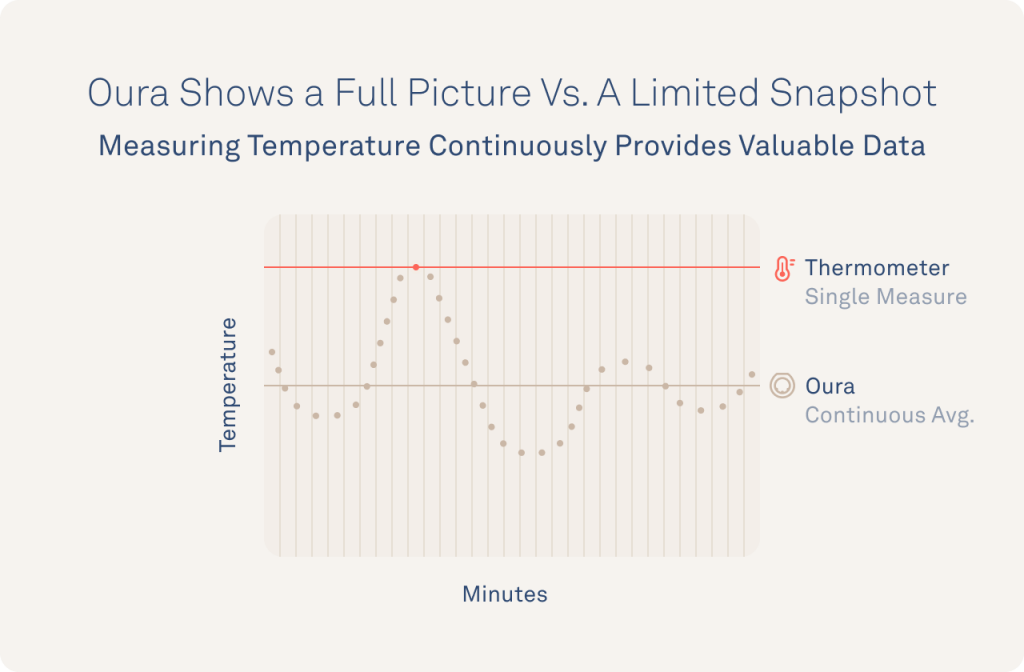
First, temperature reveals more information when it is measured every minute. Just like your heart rate, your temperature is constantly changing as your body adapts to internal and environmental changes. Measuring temperature (even multiple times a day) with an oral thermometer only measures a limited snapshot of your temperature while measuring continuously captures the full picture of changes in your body.
Second, skin temperature captures meaningful temperature variations. Your body holds your core temperature within a very narrow range, by sending heat to and from your skin (part of your body’s “shell”). This means that measuring temperature changes at sites that try to estimate your core temperature (like your mouth) will only yield small variations, ~0.5-1°C (~1-2°F) in a day. By contrast, your skin temperature changes ~15°C (27°F) or more over the course of the day and therefore captures subtle temperature fluctuations that happen minute to minute, and hour to hour.

Believe it or not, such fast, large fluctuations in skin temperature are very informative. They reflect your body’s carefully tuned temperature regulation system that allows you to maintain a fairly stable range of core temperature by redirecting heat out through your skin across the day. Your body changes the amounts and pattern of heat redirection in particular ways depending on if you are healthy or sick, male or female, asleep or awake, and more.
Researchers are already using skin temperature to advance our understanding of a wide range of subjects including identifying REM1 and sleep quality2,3, fever detection4, and menstrual cycle monitoring.5,6

Additionally, the Oura Ring is uniquely suited to collect high quality temperature data due to its innovative design:
- Precise sensors: The Oura Ring packs a sophisticated NTC temperature sensor that can account for temperature changes inside of the hardware while precisely measuring from your skin.
- Form factor: The form factor maintains ideal skin contact by surrounding your finger, unlike wrist-based sensors which tend to lose contact with your skin, compromising data quality.7
- Battery design: The Oura Ring is engineered to maintain continuous data collection at a high sampling rate, over multiple days, without straining the battery.
The Validation
Oura’s Science Team assembled a task force of employees, data scientists, physiologists, and engineers to fast-track publicly available validation results. In total, the team was able to collect 93,571 data points in a single week.
The task force selected iButton sensors as the research-grade tool to evaluate Oura’s performance.8 The goal of this study was not only to validate Oura’s temperature sensor under lab conditions, but to show that Oura maintains performance even during the challenges of measuring data in ‘noisier’ real-world scenarios.
Note: This validation included the enabling of daytime temperature data collection for research purposes. Daytime temperature readings are not currently available inside the Oura App.
Here was the protocol:
- Lab Conditions: To evaluate Oura’s temperature sensors purely as measurement tools, Oura Ring was tested in isolation (not on fingers) against 7 iButtons in temperature-controlled water baths. They were tested at precise temperature rates and ranges that were designed to cover the full physiological range of skin temperatures from extremely low (9°C [48°F], determined from Oura data in Antarctica) to very high (45°C [81°F], slightly over the maximum temperature a human can withstand during fever and survive).
- Real-World Conditions: 16 individuals spent a week wearing Oura Ring alongside 5 iButton sensors strapped to their fingers, wrists, arms, abdomen, and clothing 24/7.
The Results
Analyzing the data confirmed that Oura’s temperature sensor:
- Matches research-grade performance under lab conditions
- Remains precise in real world conditions
- Reflects changes in your physiology, not your environment
You can follow along with these findings below.
Oura’s Temperature Sensor Matches Research-Grade Performance Under Lab Conditions
Results revealed that the Oura Ring temperature measurements matched research-standard iButton performance (r² >0.99), measured changes as precisely as 0.13°C (0.234°F), and were accurate to within 0.36°C (0.648°F).
Oura’s Temperature Sensor Remains Highly Accurate And Precise In Real World Conditions
To evaluate Oura’s temperature sensors “in the wild,” 16 individuals wore both iButton and Oura Ring for a week of real world data collection on the same finger. These individuals were able to show that Oura continued to match performance with iButtons (r² >0.92) throughout the full spectrum of life events including exercising, showering, cooking, working, and everything in between.
Below is an example of how closely Oura and iButtons on the finger track across two individuals for two example days from the experiment.

Oura’s Finger Temperature Reflects Your Physiology – Not Your Environment
Because your finger is part of your body’s skin (your “shell”) and not your core, it can change temperature much more dramatically, and much faster than places that approximate your core temperature, like your mouth. However, some people express concern that measuring from your skin temperature might be capturing changes in your surrounding environment, rather than your body.
In reality, changes in your skin temperature reveal meaningful information about how your body responds to your surroundings that is separate from your environment’s temperature..
For example, imagine plunging your hands into the snow to make a snowman. Even if you put your whole hand into the snow, your fingers feel noticeably colder than your wrists. Although our environment impacts our body’s temperature, your fingers aren’t just ‘measuring’ the temperature of the snow, they are actually reflecting what is happening inside your body as blood flow changes uniquely from your fingers, wrist, and other parts of your shell so your body can maintain your core temperature.
To confirm that finger temperature captures unique physiological changes, the team analyzed the difference between iButton sensors on the finger as well as an ‘environmental sensor’ that traveled with participants to measure the world around them as they went about their days.
Results show that while the Oura Ring and finger iButton match 92% (r²=0.92), temperature information from the finger is uncorrelated to the environmental temperature; 0.1% (r²=0.001).
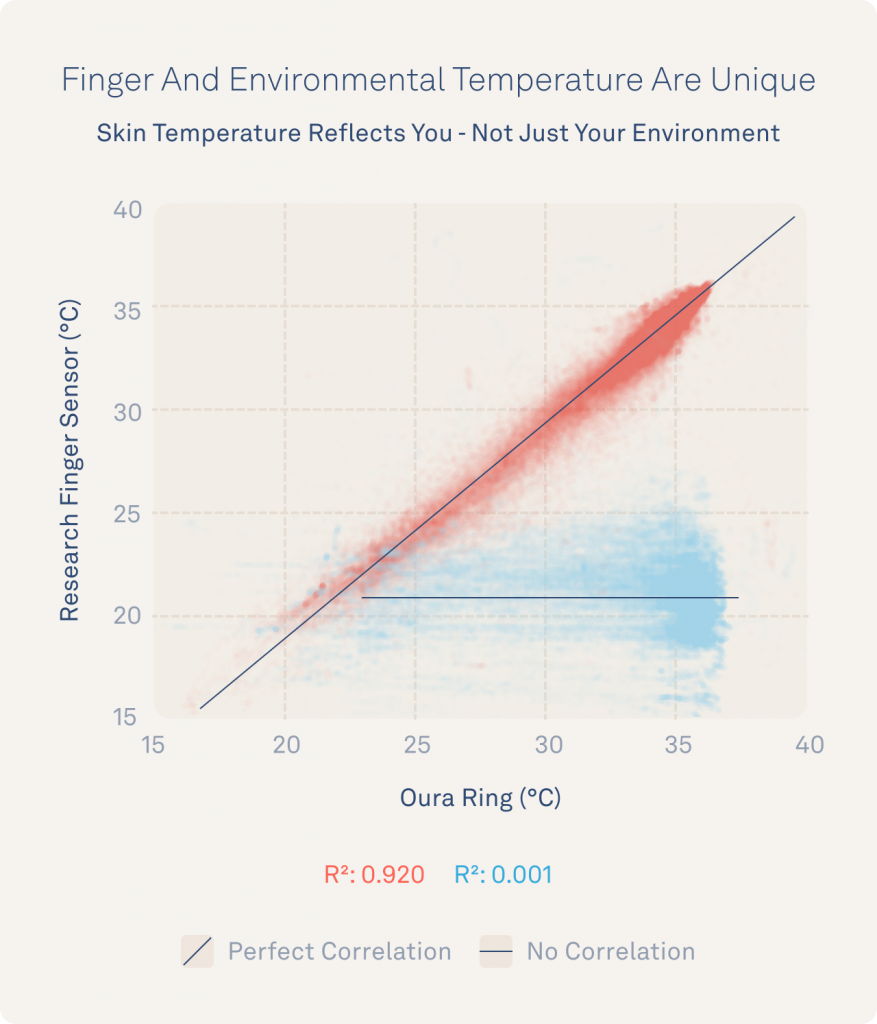
Although our environment helps our brain make decisions about how to thermoregulate, it isn’t directly determining your finger temperature all by itself. This builds even greater confidence that Oura temperature is reflecting you, not your surroundings and that many factors, including time of day, your stress levels, your hormones, your activities, and your sleep contribute to this unique signal.
Below are two examples of the clear difference between Oura Ring temperatures and environmental temperatures surrounding these individuals throughout their days.

What’s Next?
Our team is always improving the tools that we offer in the hopes that consumers and researchers will discover more about our health. The Oura temperature signal is already proving useful for real-world applications like fever detection and menstrual cycle tracking.
Continuous skin temperature data has an incredible amount of potential to provide insights into our own health as well as a tool for advancing research. We hope to continue to share our work and collaborate with you as we discover new patterns.
Read More:
- Why Oura Measures Temperature from Your Finger
- Your Normal Body Temperature Isn’t Just 98.6 Degrees
- Your Body Temperature & Oura
References
- Henane, R., Buguet, A., Roussel, B. & Bittel, J. Variations in evaporation and body temperatures during sleep in man. J. Appl. Physiol. 42, 50–55 (1977).
- Weiss, N., Attali, V., Bouzbib, C. & Thabut, D. Altered distal-proximal temperature gradient as a possible explanation for sleep-wake disturbances in cirrhotic patients. Liver Int. Off. J. Int. Assoc. Study Liver 37, 1776–1779 (2017).
- Garrido, M. et al. Abnormalities in the 24-hour rhythm of skin temperature in cirrhosis: Sleep-wake and general clinical implications. Liver Int. Off. J. Int. Assoc. Study Liver 37, 1833–1842 (2017).
- [Preprint] Smarr, B., Aschbacher, K., Fisher, S. M., Chowdhary, A., Dilchert, S., Puldon, K., … & Mason, A. E. (2020). Feasibility of continuous fever monitoring using wearable devices.
- Maijala, A., Kinnunen, H., Koskimäki, H., Jämsä, T. & Kangas, M. Nocturnal finger skin temperature in menstrual cycle tracking: ambulatory pilot study using a wearable Oura Ring. BMC Womens Health 19, 150 (2019).
- [Preprint] Grant, A. D., Newman, M. & Kriegsfeld, L. J. Ultradian Rhythms in Heart Rate Variability and Distal Body Temperature Anticipate the Luteinizing Hormone Surge Onset. bioRxiv 2020.07.15.205450 (2020) doi:10.1101/2020.07.15.205450.
- [Preprint] Smarr, B., Aschbacher, K., Fisher, S. M., Chowdhary, A., Dilchert, S., Puldon, K., … & Mason, A. E. (2020). Feasibility of continuous fever monitoring using wearable devices.[Preprint] Grant, A. D., Newman, M. & Kriegsfeld, L. J. Ultradian Rhythms in Heart Rate Variability and Distal Body Temperature Anticipate the Luteinizing Hormone Surge Onset. bioRxiv 2020.07.15.205450 (2020) doi:10.1101/2020.07.15.205450.
- Hasselberg MJ, McMahon J, Parker K. The validity, reliability, and utility of the iButton® for measurement of body temperature circadian rhythms in sleep/wake research. Sleep Med. 2013;14(1):5-11. doi:10.1016/j.sleep.2010.12.011Used in 92+ Studies in Pubmed as of 9.17.20. (link)




