- Fluctuations in your menstrual cycle are natural and occur in response to a range of factors, including training, stress, and health conditions.
- These changes are typically not a cause for concern, and a few lifestyle adjustments can help you regain balance.
- Using Oura can empower you to detect significant changes in your cycle and identify the possible root causes.
Your menstrual cycle provides crucial insights into your hormonal health. Hormones are chemical messengers that control every process in your body — from your menstrual cycle to your circadian rhythm — so keeping them balanced is essential for whole-body health.
Your menstrual cycle can also be seen as a “litmus test” for your overall health, notes Neta Gotlieb, PhD, Product Manager, Reproductive Health at Oura and clinical research scientist. In fact, your cycle is considered by many to be the “fifth vital sign” — along with body temperature, heart rate, respiratory rate, and blood pressure — that provides insights in your overall health.
What is the Average Menstrual Cycle Length?
Most people assume the average menstrual cycle length is 28 days — however, research shows that only 13% of people have a regular 28-day cycle, and the actual average is 29.3 days. A normal cycle — beginning on the first day of your period and ending on the first day of the next — can last anywhere from 21 to 35 days, while your period can last from two to seven days.
According to anonymized Oura data, the typical number of days between period onset and ovulation for Oura members ranges from about 8 days up to 25 days. Read more here about how Oura scientists busted the 14-day ovulation myth.
Noticing that your cycle is getting shorter? Many people experience natural variations in cycle length — it could be 26 days one month and 33 the next. So the first thing to ask is: is this normal for you? If your cycles have always been short, there’s nothing to worry about — that’s just your body’s natural rhythm.
However, if your body usually runs like clockwork and you notice a sudden change or your cycle becomes consistently shorter over several months, there may be hidden causes behind it.
| Member Tip: Detect changes in your cycle by using Oura’s Cycle Insights feature. This feature gives you insights into your average cycle length, period length, and the variability in your cycle. |
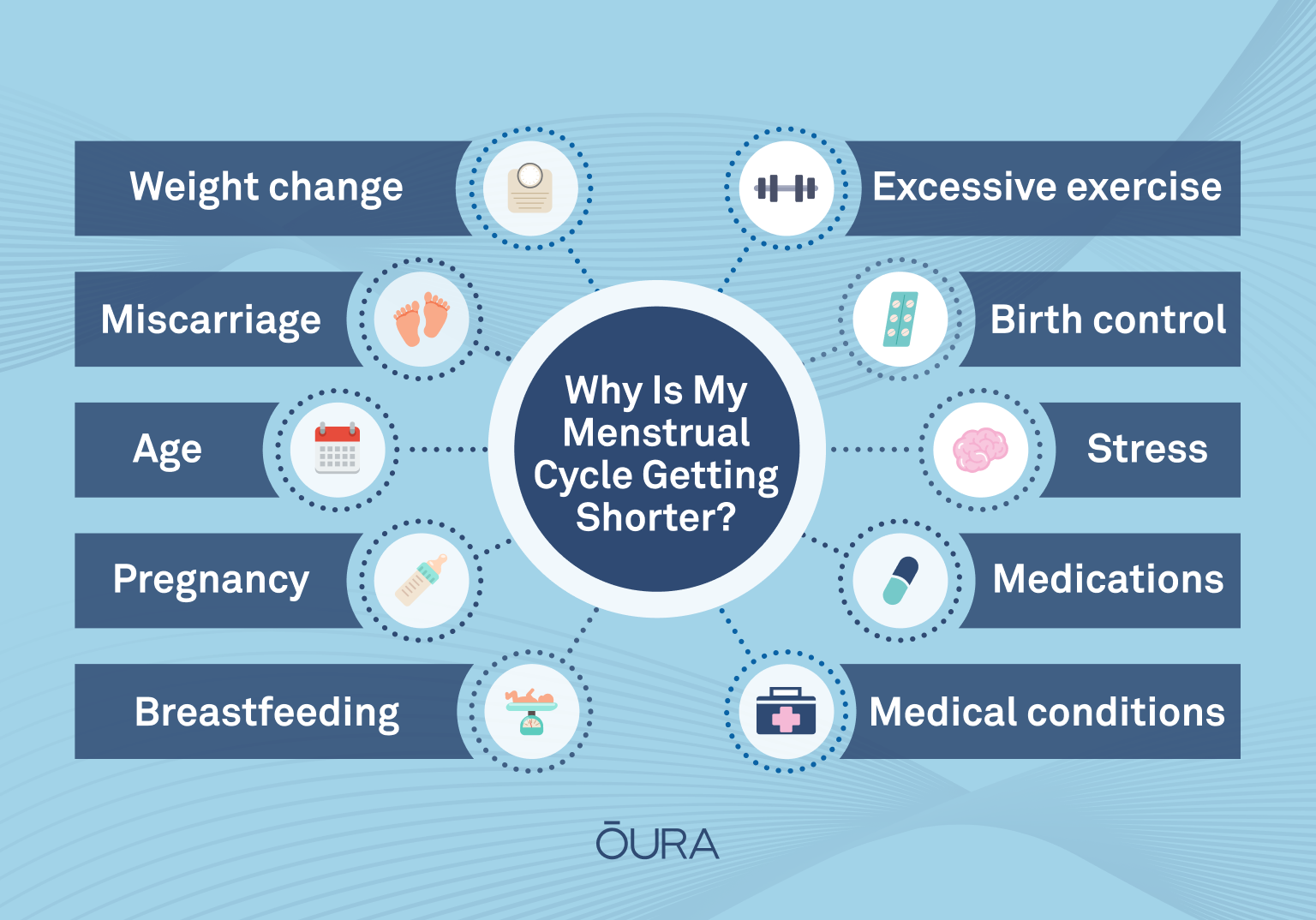
7 Possible Reasons Why Your Period is Getting Shorter
Many factors can influence the length of your menstrual cycle, including hormonal fluctuations and underlying health issues. Let’s take a look at seven of the most common causes.
1. Age
A woman’s body changes throughout her life, and hormonal changes at different life stages can affect the length of her cycle. For instance, girls going through puberty often experience irregular cycles. This is because their bodies have not yet established a regular pattern. It’s also common for teenagers to have anovulatory cycles (a cycle when no ovulation occurs). Most women find that as their bodies mature, their cycles settle into a pattern and become more predictable.
In most cases, this will last until you hit perimenopause, when hormonal changes can cause your menstrual cycles to become shorter. This is the time leading up to menopause, and it usually begins when a person is in their late 30s or 40s.
During perimenopause, the ovaries produce less of the hormone estrogen, causing menstrual cycle changes such as shorter cycles, lighter or heavier flow, or skipping periods entirely. Impaired sleep is also a sign of perimenopause, and other symptoms may include hot flashes, insomnia, night sweats, and vaginal dryness.
READ MORE: How Does Menopause Affect Sleep?
2. Pregnancy, Miscarriage, or Breastfeeding
If you have a period that is much shorter or lighter than usual, there’s a chance it’s not actually a period but implantation bleeding, a symptom of early pregnancy. It occurs in about 15 to 25 percent of pregnancies when a fertilized egg attaches itself to the uterine lining, causing light bleeding that’s easy to mistake for a period.
Similarly, if you miscarry during the very early stages of pregnancy, you might not even know you’re pregnant and mistake the subsequent bleeding for your period.
If you’re breastfeeding, the hormone prolactin — which helps you produce breast milk — interferes with your menstrual cycle. This is why most women don’t get their periods back right away after giving birth. Quick PSA, though: Breastfeeding doesn’t “protect” against getting pregnant, Gotlieb reminds us, and shouldn’t be considered a contraceptive.
Plus, when your period does come back, prolactin can make it shorter and lighter than usual.
3. Stress
When you’re under acute stress, your body releases the epinephrine (aka adrenaline), which is the fight-or-flight hormone. Once the stressor passes, cortisol levels subside, and balance is restored.
However, if the stress is chronic (i.e., goes on for a long period of time), your cortisol levels can remain elevated, disrupting the delicate hormonal balance in your body and causing irregularities in your cycle that can make them shorter.
| Member Tip: If you think stress could be contributing to shorter menstrual cycles, track your stress levels on Oura with Daytime Stress. |
4. Weight Change
Both losing and gaining weight can affect your body and cycle in a number of ways. For instance, losing a lot of weight rapidly puts the body under stress, which can make cortisol levels shoot up and cause shorter menstrual cycles.
On the other hand, adipose (fat) tissue releases the hormone estrogen, which plays a key role in regulating your cycle. Therefore, gaining weight can cause an excess of estrogen that can throw your cycles out of whack, as can excessive weight loss because your body needs at least 22% body fat to menstruate properly.
Additionally, eating disorders like anorexia nervosa or bulimia nervosa, can shorten your menstrual cycle or cause periods to stop altogether.
5. Excessive Exercise
Studies have shown that excessive exercise can create hormonal imbalances that cause irregular or short menstrual cycles. While getting regular exercise is important for maintaining overall health, it’s essential to adapt your routine to your body’s needs to avoid overtraining.
Strenuous exercise is a form of stress, which releases the hormone cortisol (are you noticing a theme here?) that can interfere with your cycle. Additionally, if you’ve started a new, lower-calorie diet to accompany your fitness regimen, you may be in a nutritional deficit. Women’s bodies are especially sensitive to nutrient depletion, and research shows that even reducing your calorie intake to 1,200 calories per day can cause a significant increase in cortisol levels.
| Member Tip: Your daily Readiness Score in the Oura App can help you plan your training schedule according to your body’s needs. For instance, if your Oura Ring detects a higher-than-normal body temperature or resting heart rate in the second part of your cycle, it may suggest a lower Activity Goal for the day so you can give your body the rest it needs, or consider using Rest Mode as a reminder to take it easy. |

RELATED: How to Align Your Training with Your Menstrual Cycle
6. Medical Conditions
Numerous health conditions — such as polycystic ovarian syndrome (PCOS), thyroid disorder, or premature ovarian insufficiency (POI) — can all lead to shorter periods.
PCOS can cause irregular menstrual periods since monthly ovulation is not occurring and androgen levels are elevated, Gotlieb explains. As a result of this imbalance of sex hormones, eggs don’t always mature or get released from the ovary to be fertilized. Instead, they collect on the ovaries as small, immature follicles, which are sometimes called cysts.
Thyroid disorders like hypothyroidism can cause your body to produce too little thyroid hormone. Since this hormone plays a vital role in your menstrual cycle, an imbalance can cause a shorter-than-usual cycle.
POI occurs when a woman’s ovaries stop releasing mature eggs before age 40, which can lead to irregular and/or light periods, similar to menopause.
7. Birth Control and Medications
If you use hormonal birth control, such as the pill, your “periods” are not real periods because the hormones in the pill prevent you from ovulating. The bleeding you experience is known as a “withdrawal bleed” that occurs when you stop taking the pill each month. (This can also occur in perimenopause, Gotlieb notes.)
The subsequent drop in hormones causes your body to shed the lining of the uterus, and many women notice their periods are lighter and shorter on birth control.
Certain medications can also interfere with your menstrual cycle. For instance, research shows that some types of antidepressants can increase levels of the hormone prolactin — which, as you may remember, can mess with your menstrual cycle.
When to Seek Medical Advice
Many factors can cause fluctuations in your cycle throughout your lifetime. In most cases, these changes are no cause for concern, and you can restore balance by managing your stress levels, diet, exercise regimen, and other lifestyle factors.
However, if you suspect there’s another underlying problem affecting your menstrual health, it may be time to seek medical advice. Consult your healthcare provider if you experience any of the following:
- Periods that become irregular after being regular
- Menstrual blood flow that contains large blood clots
- Pelvic pain or bleeding when not menstruating
- Particularly heavy bleeding
- Missing a period for three months
| Member Tip: Show your doctor your Cycle Report, accessible within the Oura App. This shareable PDF report of your cycle data generated by the Oura App, offers key insights into your cycle phases, temperature trends, period length, and logged symptoms that can be invaluable information in a medical setting. |
The Bottom Line: Why Is My Menstrual Cycle Getting Shorter?
If you’ve been asking yourself, “why is my menstrual cycle getting shorter?” know that fluctuations are often a normal part of life. Women’s health expert, Neta Golieb, PhD explains that common factors like age, stress, exercise, and hormonal changes can all play a role — and in most cases, shorter cycles aren’t a cause for concern. Still, consistent changes in your cycle may signal an underlying condition that deserves attention.
With Cycle Insights in the Oura App, you can track your average cycle length, spot trends over time, and connect the dots between lifestyle habits and menstrual changes. By combining personal awareness with data, you’ll be better equipped to understand what’s normal for your body — and when it might be time to check in with a healthcare professional.
RELATED: How Your Menstrual Cycle Impacts Your Entire Body
About the Oura Expert
Neta Gotlieb, Ph.D., is a Lead Clinical Research Scientist at ŌURA researching and developing solutions focused on women’s health. Her mission and passion is to solve challenges related to reproductive health and empower ŌURA users to make informed, data-driven decisions. Before joining ŌURA, she worked at a nonprofit organization as their Head of Volunteering Programs, but her passion for scientific discovery inspired her to pursue a career as a research scientist. Gotlieb received her Master’s degree from Tel Aviv University in Biological Psychology where her work focused on how stress impacts immune function. She then earned a PhD from UC Berkeley where she studied Reproductive Endocrinology and the circadian regulation of menstrual cycles, pregnancy, and birth. Outside of work, Neta enjoys hiking, biking, and spending time with her family. She lives in the Bay Area with her husband and two children.











