Globally, approximately 49% of women of reproductive age (from 15 to 49 years) use some form of contraception, or birth control.
There are two main categories of birth control: hormonal and non-hormonal. Hormonal birth control options include birth control pills and progesterone implants. Non-hormonal birth control options include fertility awareness methods, such as with the Natural Cycles app powered by Oura, and the copper IUD.
| Member Tip: Try Natural Cycles, powered by Oura, for an all-natural, FDA-cleared contraception option. |
While there are key differences between hormonal and non-hormonal birth control, know that there’s no one-size-fits-all option. Above all, it’s important to inform yourself when deciding which birth control is best for you.
“Empowerment comes from knowledge,” says Dr. Neta Gotlieb, Senior Product Manager of Women’s Health at Oura. “Every choice you make about your body and reproductive health is deeply personal and should be guided by a clear understanding of how it aligns with your unique needs and goals. You know your body best, and being informed about how different birth control options fit into your life can help you make the decisions that are right for you.”
Keep reading to learn more, and always speak to your healthcare provider to find the method that’s right for you.
RELATED: How Your Menstrual Cycle Impacts Your Entire Body
What Is Hormonal Birth Control?
Common hormonal birth control methods include an intrauterine device (IUD), birth control pill, and patch. They rely on synthetic hormones—usually estrogen, progesterone, or a combination of both—to regulate the menstrual cycle and prevent pregnancy.
The combination of these hormones prevents pregnancy in different ways depending on the type. They may prevent ovulation (the release of an egg), thicken cervical mucus to block sperm, or alter the uterine lining to prevent implantation.
Effects of Hormonal Birth Control
Hormonal birth control has been extensively studied to understand its potential benefits and drawbacks.
Potential Benefits
- High efficacy: Overall, hormonal birth control is highly effective. Studies show effectiveness varies from 91 to 99% in preventing pregnancy.
- Reduced premenstrual symptoms: Many women (more than 90%!) experience symptoms of premenstrual syndrome (PMS) like bloating and fatigue. Others may experience premenstrual dysphoric disorder (PMDD), which has more severe symptoms like depression and anxiety. Some research suggests that hormonal birth control can help mitigate these symptoms for some individuals.
- Lighter and more regular periods: Because hormonal birth control can help balance the hormonal fluctuations that happen throughout the cycle, it tends to make periods lighter and more consistent in their timing.
- Manage certain health conditions: Regulating your hormones and your cycle can help to reduce symptoms of health conditions such as polycystic ovary syndrome (PCOS), endometriosis, and perimenopause.
- Fewer migraines: Some types of hormonal birth control have been shown to ease migraine pain for women who experience them.
- Lower risk of certain cancers: Hormonal birth control has been associated with a decreased risk of uterine, ovarian, endometrial, and colorectal cancer. In fact, women who take combination birth control pills are 50 percent less likely to get uterine cancer.
Potential Risks
- Increased mood changes: Synthetic hormones can alter the balance of neurotransmitters in the brain, which regulate emotions and mood. While some research has found that women taking the pill had an increase in negative mood and anxiety, the research is mixed. One review of studies concluded that women with underlying mood disorders may be at greater risk when taking hormonal birth control, but most women do not experience mood changes.
- Headaches and migraines: Research has shown a link between hormonal birth control and headaches or migraines.The reason: Synthetic hormones can alter your natural estrogen levels, which in some cases can trigger headaches.
- Altered sleep patterns: Because estrogen regulates the circadian rhythm, some women may experience changes in their sleep when they use hormonal birth control. For some, particularly premenopausal women, sleep improves. However, for women of reproductive age, there’s an association between hormonal birth control and insomnia, daytime sleepiness, lower sleep quality, and increased sleep duration (possibly due to increased tiredness).
- Increased risk of cardiovascular disease (CVD): Hormonal contraceptives have been associated with an increased risk of CVD. Because natural estrogen helps to regulate blood thickness, synthetic estrogen impacts this balance, which can lead to CVD.
- Vitamin deficiencies: Studies have shown that hormonal contraceptives can deplete certain essential vitamins, due to the effect of synthetic hormones on nutrient absorption and metabolism.
- Increased risk of certain cancers: Hormonal birth control, particularly long-term use, has been linked to an increased risk of breast and cervical cancer. However, this increased risk is relatively low—for hormonal IUDs, it’s about 14 additional breast cancer diagnoses for every 10,000 women.
Types of Hormonal Birth Control
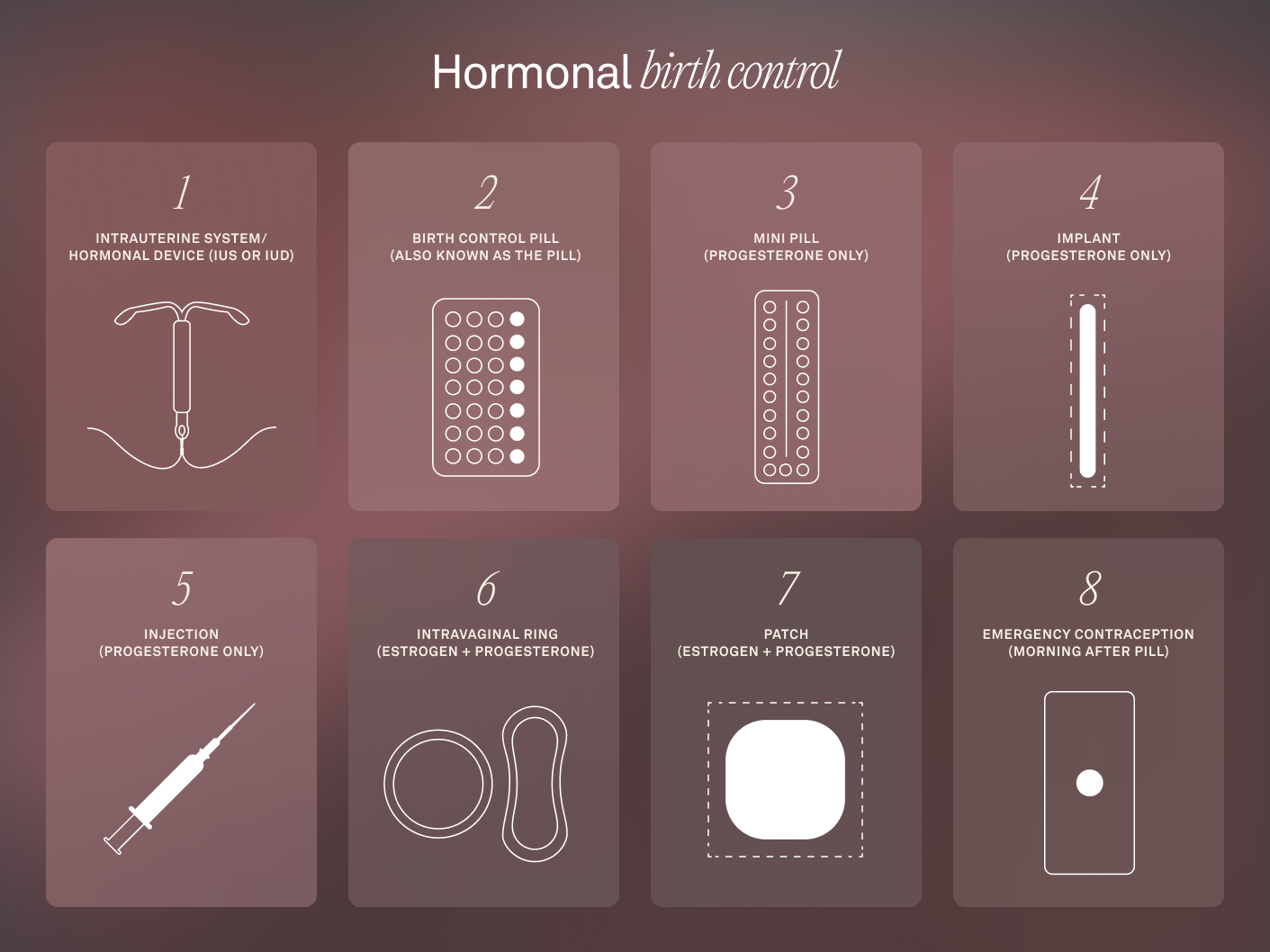
1. Intrauterine System/Hormonal Device (IUS or IUD)
The hormonal IUS/IUD is a small T-shaped device inserted into the uterus by your doctor. It continuously releases a low dose of progestin (a synthetic form of progesterone) that thickens cervical mucus and thins the uterine lining, making it more difficult for sperm to reach the egg.
Usage: Once inserted by a doctor, IUS/IUD is a long-acting, reversible contraceptive that can last anywhere from 3 to 5 years.
Effectiveness: 99%
Impact on Cycle: Cycle length may change. Can reduce or stop ovulation depending on the brand and the amount of synthetic progesterone released. Period may be irregular or light; possibly no bleeding.
Impact on Body Temperature: Marginal temperature elevation, no cyclical changes
2. Birth Control Pill (also known as the Pill)
This is the most common hormonal birth control method, used by 14% of women in the United States and 9% of women globally. It’s a once-daily pill that contains synthetic versions of the hormones estrogen and progesterone. It works by preventing ovulation (the release of an egg from the ovary), thickening cervical mucus, and thinning the uterine lining, making it difficult for sperm to reach an egg.
Usage: You’ll take the pill orally for 21 days, followed by a 7-day break (either via placebos or by not taking any pills) during which a withdrawal bleed (period) occurs.
Effectiveness: Perfect use: 99%; typical use: 93%
Impact on Cycle: Stops natural cycle and suppresses ovulation. No “period,” but predictable withdrawal bleeding during hormone-free days.
Impact on Body Temperature: Marginal temperature elevation, no cyclical change
3. Mini Pill (Progesterone Only)
The mini pill contains only progesterone, which works by thickening cervical mucus and altering the uterine lining, making it more difficult for sperm to reach an egg. In some cases, the mini pill also prevents ovulation, but this effect is not as consistent as with the birth control pill.
Usage: The mini pill must be taken at the same time each day, with no breaks between doses.
Effectiveness: Perfect use: 99%; typical use: 92%
Impact on Cycle: Stops natural cycle, but may not suppress ovulation. Periods may be irregular or reduced, or no bleeding.
Impact on Body Temperature: Marginal temperature elevation, no cyclical changes
4. Implant (Progesterone Only)
The implant is a small, flexible rod that is inserted under the skin of the upper arm by a healthcare provider. It releases a steady amount of synthetic progesterone (progestin) into the bloodstream. This hormone works by thickening cervical mucus to prevent sperm from reaching the egg and by suppressing ovulation in many users.
Usage: Once implanted by a healthcare provider, it’s a long-acting reversible contraceptive lasting about 3 years.
Effectiveness: 99%
Impact on Cycle: Suppresses natural cycle and ovulation. Periods may be irregular or no bleeding.
Impact on Body Temperature: Marginal temperature elevation, no cyclical changes.
5. Injection (Progesterone Only)
The contraceptive injection contains progestin, a synthetic form of progesterone. It works by preventing ovulation and thickening cervical mucus.
Usage: The injection is typically administered by a healthcare provider once every three months.
Effectiveness: Perfect use: 99%; typical use: 96%
Impact on Cycle: Suppresses natural cycle and ovulation. Periods may be irregular or no bleeding.
Impact on Body Temperature: Elevated temperature, no cyclical changes
6. Intravaginal Ring (Estrogen + Progesterone)
The intravaginal ring is a flexible, transparent ring that releases both estrogen and progesterone. It is inserted into the vagina, where it remains for 3 weeks, releasing a steady dose of hormones to prevent ovulation and thicken cervical mucus.
Usage: After 3 weeks, the ring is removed for a 1-week break, during which the user experiences a withdrawal bleed (period). The ring is simple to use, but it requires the user to remember to insert and remove it on schedule.
Effectiveness: Perfect use: 99%; typical use: 93%
Impact on Cycle: Suppresses hormonal cycle and ovulation. Withdrawal bleeding occurs during hormone-free week.
Impact on Body Temperature: Marginal temperature elevation
7. Patch (Estrogen + Progesterone)
The contraceptive patch is a small adhesive patch that releases both estrogen and progesterone through the skin. It is applied to the skin (usually on the arm, back, or abdomen) for 3 weeks, followed by a 1-week break to allow for a withdrawal bleed.
Usage: Like the pill and the ring, the patch works by preventing ovulation and thickening cervical mucus. It’s important to replace the patch weekly and ensure that it stays adhered to the skin.
Effectiveness: Perfect use: 99%; typical use: 92%
Impact on Cycle: Suppresses hormonal cycle and ovulation, with bleeding during hormone-free week.
Impact on Body Temperature: Marginal temperature elevation, no cyclical change
8. Emergency Contraception (Morning After Pill)
The morning after pill is used to prevent pregnancy after unprotected sex or contraceptive failure. It contains progestin or a combination of hormones and works by delaying or preventing ovulation. Note that it does not prevent pregnancy after conception; only before ovulation by preventing ovulation. This means that if conception has occurred, it will not work.
Usage: The pill must be taken within 72-120 hours of unprotected sex for maximum effectiveness. It is not intended for regular contraception but rather as an emergency option. It may cause temporary disruptions to the menstrual cycle.
Effectiveness: 95% effective if you take it within 24 hours (1 day) of unprotected sex. 85% effective if you take it within 25-48 hours (2 days) and 58% effective if you take it within 49-72 hours (3 days). Lower effectiveness at 4-5 days.
Impact on Cycle: Disrupts the cycle and suppresses ovulation. Bleeding between periods or heavier menstrual bleeding may occur.
Impact on Body Temperature: May increase body temperature for 1-2 days, longer-term impact is unlikely.
Do You Have a Period on Hormonal Birth Control?
On hormonal birth control, the bleeding you experience is typically withdrawal bleeding, not a true menstrual period. It happens when you stop taking hormones, like during the hormone-free days of the birth control pill, patch, or intravaginal ring. This bleeding mimics a period, but results from the drop in hormones, not from ovulation.
| Member Tip: If you’re on a hormonal birth method, know that your cycle is not in a predictable biometric-based pattern. Therefore, we do not recommend using Oura’s Cycle Insights feature. You can still learn more about how your body changes throughout the month by tracking certain metrics such as body temperature trends, HRV, and heart rate. Learn more here. |
What Is Non-Hormonal Birth Control?
Non-hormonal birth control options include the fertility awareness method—for example, Natural Cycles, powered by Oura—the copper IUD, and cervical cap.
All of these methods work differently, but have one thing in common: They don’t utilize hormones to prevent pregnancy, and allow your body to experience a natural menstrual cycle. These methods also vary in effectiveness, especially in terms of typical use effectiveness.
| Member Tip: If you’re on non-hormonal birth control, you can opt into Oura’s Cycle Insights, which provides helpful data and personalized insights during every cycle phase. |
Types of Non-Hormonal Birth Control

1. Temperature Tracking Methods
How it works: These methods monitor changes in your basal body temperature (BBT) to identify fertile and non-fertile days. After ovulation, your body temperature rises slightly, signaling that the fertile window has passed. By tracking these daily temperature shifts, users can avoid unprotected sex on fertile days to prevent pregnancy.
One example of this method is Natural Cycles, the only FDA-cleared birth control app that analyzes body temperature and other key fertility indicators to calculate daily fertility status. In NC° Birth Control mode, users receive “Green Days” to indicate that a user is unlikely to be fertile and can have unprotected sex and “Red Days” to indicate when a user may be fertile and should use protection or abstain from sex if trying to prevent pregnancy.
Usage: Your temperature is measured every morning before getting out of bed and input into the app for analysis. You can also wear Oura Ring to sleep and your overnight temperature trends from the ring will sync with the NC° app in the morning.
Effectiveness: For Natural Cycles: perfect use: 98%; typical use: 93%. (Reference: Contraceptive Technology [Table 26 – 1]. 21st Edition, 2018)
| Member Tip: Use Natural Cycles, powered by Oura to sync your temperature automatically. Sign up for your exclusive 28-day free trial here. |
2. Copper IUD
How it works: The copper IUD is a small, T-shaped device inserted into the uterus. It releases copper ions that are toxic to sperm, preventing fertilization. The copper IUD also alters the uterine lining, making it less hospitable for a fertilized egg to implant. It does not involve hormones.
Usage: A healthcare provider inserts the IUD into the uterus during a quick procedure.
Effectiveness: 99%
3. Cervical Cap
How it works: The cervical cap is a small, flexible silicone or rubber cup that fits over the cervix, blocking sperm from entering the uterus.
Usage: The cap is inserted into the vagina before intercourse, left in place for up to 6 hours, and removed afterward.
Effectiveness: Perfect use: 92-96%; typical use: 71% in people who have given birth, 86% in those who haven’t
How Non-Hormonal Birth Control Impacts Your Body
Non-hormonal birth control methods allow your body to maintain a natural menstrual cycle since they don’t rely on synthetic hormones. However, your menstrual cycle still affects your entire body.
The start of your period marks day one of your cycle and the start of the follicular phase. This phase includes menstruation and helps your body prepare to release an egg or ovulate. Many women feel energized during the follicular phase, thanks to biometric changes such as a lower resting heart rate, higher HRV, and lower body temperature.
Once you ovulate, you shift into the luteal phase. In this phase, higher levels of progesterone raise your body temperature, while HRV typically declines and resting heart rate may increase. If the egg released isn’t fertilized, progesterone and estrogen drop, triggering menstruation. During this time, people may experience symptoms of premenstrual syndrome (PMS), such as fatigue, bloating, and mood swings.
While some women may not be affected by these hormonal fluctuations, others may experience significant impacts on their mood and well-being. This is known as premenstrual dysphoric disorder (PMDD), which affects about 5 to 8% of women. In these cases, hormonal birth control may be advised as a way to reduce symptoms.
RELATED: Cycle Syncing 101: Support Your Sleep, Mood, and Energy Throughout Your Cycle
About the Oura Expert
Dr. Neta Gotlieb, is a Product Manager and Clinical Research Scientist who’s driven by a desire to support women with intuitive, useful features and easy-to-understand data and insights. At Oura, Dr. Gotlieb has led the teams who developed innovative women’s health features, such as Cycle Insights and Pregnancy Insights. Dr. Gotlieb earned a Master’s Degree in Biological Psychology from Tel Aviv University and a PhD in Reproductive Neuroendocrinology from University of California Berkeley, where she focused on the neural regulation of menstrual cycles, pregnancy, and birth. She has also received the Women in Tech Global Technology Leadership Award. A mother of two daughters, Dr. Gotlieb is the author of the children’s book, Every Body’s Brain.











