Snoring is a common condition, with about 45% of adults experiencing occasional snoring. In many cases, this is harmless. However, regular snoring can be a sign of something more serious like sleep apnea, a sleep disorder that occurs when breathing stops and starts repeatedly during sleep. Anyone can develop sleep apnea, but there’s a growing link between regular menopause and sleep apnea that needs to be investigated.
Oura members can use the blood oxygen sensing (SpO2) feature to measure their blood oxygen saturation levels and variations. This feature can monitor breathing disturbances during sleep and show how well your body absorbs and circulates oxygen.
While sleep apnea is more prevalent in males, women’s risk of developing sleep apnea increases after menopause. According to Grace Pien, MD, assistant professor of medicine at the Johns Hopkins Sleep Disorders Center, postmenopausal women are two to three times more likely than premenopausal women to have sleep apnea.
In addition, women who develop sleep apnea after menopause tend to experience more severe symptoms compared to younger women. One big reason behind this is hormonal changes in women as they get older.
The Impact of Menopause on Hormones
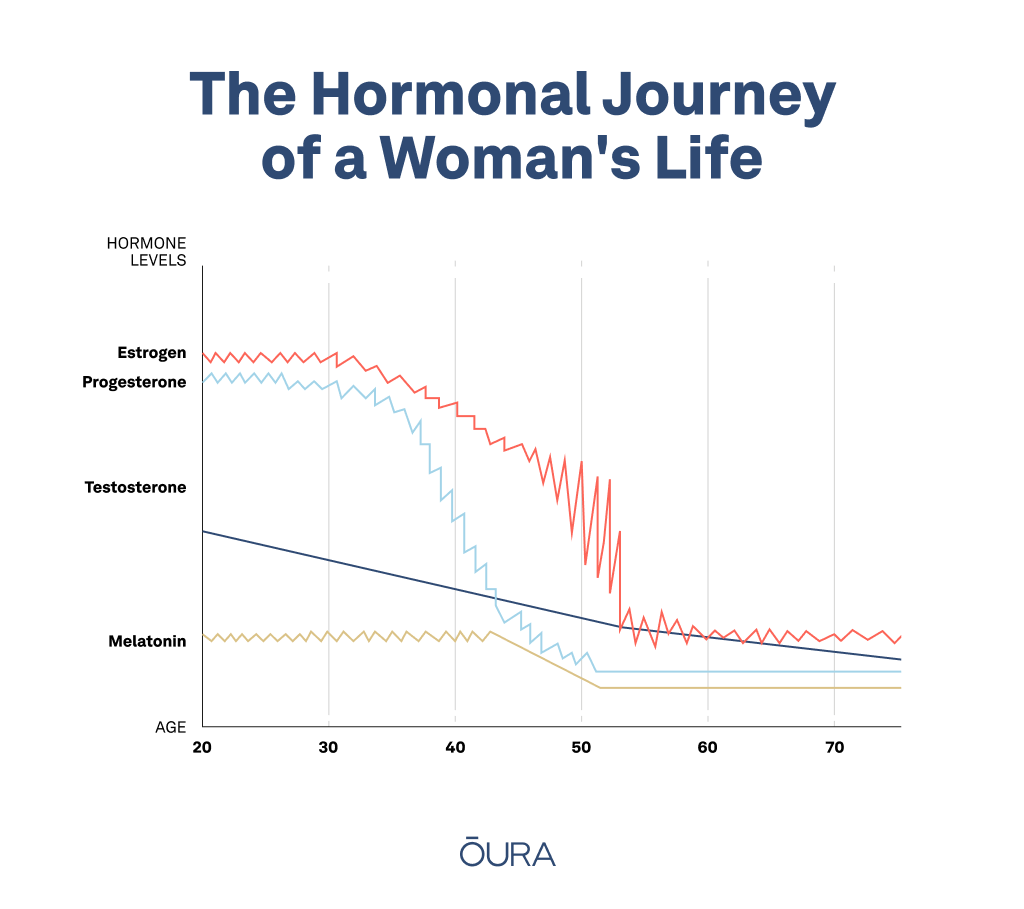
Menopause typically occurs 12 months after a woman’s last period — or between the ages of 45 and 55. This time is characterized by a series of physiological changes that are triggered by a decline in the production of female hormones.
These hormones are responsible for regulating a wide range of bodily functions, including the menstrual cycle, bone density, and brain function. As such, when a woman enters menopause, her body undergoes a series of hormonal changes that can have significant consequences for her health and well-being. To name a couple:
- A decrease in estrogen and progesterone production is one of the most significant hormonal changes that occur during menopause. These hormones play critical roles in a woman’s reproductive system, and their deficiency can cause a variety of symptoms including hot flashes, night sweats, mood swings, and vaginal dryness.
- Moreover, a drop in estrogen and progesterone levels also increases the likelihood of snoring in women. One study found that middle-aged women with low levels of estrogen and progesterone are more likely to experience snoring and other symptoms of obstructive sleep apnea, as not everyone experiences snoring. Other signs of sleep apnea include dry mouth or headache in the morning, or gasping for air.
The Connection Between Menopause & Sleep Apnea
Menopause and the physiological changes that occur during it can influence the likelihood of both milder conditions such as snoring, and more serious conditions such as sleep apnea.
As estrogen levels decline during menopause, there is a decrease in muscle tone in the upper airway, including the tongue, soft palate, and throat muscles. This can lead to increased airway resistance, making it more difficult to breathe during sleep, and causing a higher likelihood of snoring and sleep apnea.
Menopausal women may also experience weight gain or changes in body fat distribution, which can contribute to sleep apnea. Excess weight around the neck and throat area can narrow the airway and make it more difficult to breathe during sleep.
In one study, researchers investigated the relationship between menopause and snoring in a sample of postmenopausal women. They discovered that postmenopausal women snore more than premenopausal women, with 47% to 67% of postmenopausal women having obstructive sleep apnea.
Further research has also found that women who experience surgical menopause (as opposed to natural menopause) are more likely to experience habitual snoring.
How to Mitigate the Risk of Snoring & Sleep Apnea During Menopause
On their own, the following steps cannot completely eliminate snoring and sleep apnea, but they can help reduce your risk and alleviate sleep apnea symptoms.
Avoid Alcohol and Sedatives
Alcohol and sedatives are known to have a relaxing effect on the muscles of the body, including those in the upper airway. When these muscles relax, they can cause the airway to narrow, making it more difficult to breathe during sleep. This can lead to snoring and sleep apnea. In fact, higher levels of alcohol consumption have been shown to increase the risk of sleep apnea by 25%.
Alcohol and sedatives also have a depressive effect on the central nervous system, which can further exacerbate the relaxation of the muscles in the airway. This can result in more frequent and louder snoring, as well as an increased likelihood of developing sleep apnea. Limiting or avoiding these substances can help improve sleep quality, ensuring a peaceful and uninterrupted slumber.
Sleep On Your Side
Sleeping position can improve or worsen snoring and sleep apnea symptoms. Thanks to the effects of gravity on the body, sleeping on your back can cause the tongue and soft palate to collapse to the back of your throat, blocking your airway, leading to snoring, and increasing the duration and frequency of sleep apnea.
On the other hand, sleeping on your side can help keep the airway open and encourage blood flow, reducing the likelihood of snoring and sleep apnea. Research has even shown that left-side sleeping reduces the severity of sleep apnea.
RELATED: 8 Popular Sleeping Positions: Find Out What They Mean For Your Health
Use A Humidifier
Menopausal women may experience dryness in the airway, which can exacerbate snoring and sleep apnea. Dry air in the bedroom can also cause irritation and inflammation in the airway, leading to snoring and sleep apnea. Using a humidifier in the bedroom can help keep the air moist and reduce dryness in the airway, helping you breathe better during sleeping.
Consult A Healthcare Provider
If your snoring or sleep apnea symptoms persist or are severe, it’s important to consult a healthcare provider. They may recommend treatments such as continuous positive airway pressure (CPAP) therapy or oral appliances to help improve breathing during sleep.
CPAP therapy involves wearing a mask over your nose and/or mouth while you sleep, which provides a steady stream of air pressure to keep your airway open. Oral appliances, on the other hand, are specially designed devices that help keep your airway open by repositioning your jaw or tongue.
A healthcare professional may also suggest hormone replacement therapy (HRT). This therapy involves taking medications containing estrogen and progesterone, which may help alleviate some of the hormonal changes associated with menopause that contribute to snoring and sleep apnea. In one pilot study, HRT reduced the severity of sleep apnea by 75%.
Maintain A Healthy Weight
Maintaining a healthy weight during menopause can go a long way in reducing the risk of sleep apnea. Regular exercise and a balanced diet are two of the most effective ways to maintain weight. As Dr. Pien points out, exercising regularly can help menopausal women fall and stay asleep.
Exercise strengthens the muscles that support the airway, improving its stability and lowering the risk of airway collapse during sleep. Additionally, regular exercise improves overall cardiovascular health, which can help reduce the risk of sleep apnea and other related health problems.
Practice Good Sleep Hygiene
By promoting better quality sleep, good sleep hygiene practices can help reduce sleep apnea. A regular sleep routine helps to regulate the body’s circadian rhythm, making it easier to fall and stay asleep throughout the night. Creating a sleep-friendly environment in the bedroom by keeping it cool, dark, and quiet can also aid in the promotion of better sleep.
When it comes to sleep apnea, keeping the bedroom cool is especially important because warm temperatures can cause the airway to narrow, increasing the likelihood of snoring and sleep apnea. Furthermore, reducing noise and light in the bedroom can reduce the risk of sleep interruptions, which can exacerbate the symptoms of sleep apnea.
If you’re an Oura member, you can use Tags to get measurable insights into how certain habits, changes, behaviors, and environmental factors impact your sleep quality and overall health.
RELATED: Oura Helps Me Spot Changes in My Cycle
The Oura Ring is not a medical device and is not intended to diagnose, treat, cure, monitor, or prevent medical conditions or illnesses.











