When you think about women’s health, heart disease is probably not the first medical condition to come to mind. But there are many reasons why it should.
Heart disease is the leading cause of death for women in the United States, and can affect women of any age. In fact, it’s responsible for about one in every five female deaths. What’s more, research finds women are more likely than men to die after having a heart attack.
As Oura launches new heart health features, it’s important to note that heart health impacts women and men differently — in some very surprising ways.
A Brief History of Women’s Heart Health
Throughout much of the 20th century, cardiovascular disease in women was overlooked by the wider medical community. Heart disease was considered a “man’s disease” — one that women didn’t have to worry about, as the American Heart Association (AHA) reports.
In the 1980s, the Framingham Heart Study, the first in-depth, long-term cardiovascular study in the U.S., began reporting sex-specific patterns of heart disease and noted that heart attacks were less likely to be recognized in women than in men.
This was followed by a landmark study in 2001 that highlighted the underrepresentation of women in clinical trials, leading to calls for more inclusive cardiovascular research, gender-specific guidelines for preventing heart disease, and campaigns for raising awareness.
While research and understanding of heart disease in women has made significant strides in the 21st century, there’s still much more to understand — as well as a significant gap to fill in research: According to a systematic review of cardiovascular clinical trials, women made only 27% of the studied population and only 33% of studies reported gender-based outcomes.
Below, learn seven must-know facts about heart disease in women, symptoms to be aware of, and what you can do to lower your risk.
7 Facts About Heart Disease in Women
1. Women have a higher risk of dying from cardiovascular disease than men.
While men have a greater prevalence of cardiovascular disease, women have a higher rate of mortality and a worse prognosis when diagnosed.
The reasons for these disparities are varied and complex, but some include:
- A historical lack of inclusion in clinical trials (as mentioned above)
- A lack of awareness: In 2019, only 44% of women recognized heart disease as the leading cause of death.
- Misunderstood and/or misdiagnosed symptoms of heart disease in women (more on this below)
- A lack of knowledge among physicians about heart disease in women: In a nationwide survey, only 22% of primary care doctors and 42% of cardiologists said they feel extremely well prepared to assess cardiovascular risks in women.
- Women are less likely than men to receive life-saving treatments for heart disease, including heart transplants, or be prescribed medications such as statins.
2. Heart disease symptoms in women can be different than in men.
While both men and women can experience “classic” heart disease symptoms like chest pain and shortness of breath, women’s symptoms tend to be different and may go unrecognized. This can contribute to misdiagnosis and a greater risk of death.
In fact, a study found that women are seven times more likely than men to be misdiagnosed and sent home from the hospital during a heart attack.
Whether you’re a woman or have loved ones in your life who are women, it’s important to know the unique symptoms of heart disease in women, which may include:
- Neck, jaw, shoulder, or upper back or upper abdominal discomfort
- Pain in one or both arms
- Nausea or vomiting
- Sweating
- Lightheadedness or dizziness
- Unusual fatigue
- Heartburn or indigestion
If you or someone you know is experiencing any of these symptoms, don’t be afraid to seek medical attention as soon as possible.
3. Female hormonal changes can increase cardiovascular risk.
Any event in a woman’s lifespan that dramatically impacts hormone levels can increase cardiovascular risk. For instance, during menopause, levels of estrogen — a cardioprotective hormone — drop. This is believed to be partly why women experience more cardiovascular events during and after menopause.
Menstrual cycle irregularities — in length, duration, or timing — are also associated with cardiovascular risk. This is because these changes are usually caused by hormonal irregularities.
RELATED: How Does Menopause Affect Sleep?
4. Pregnancy may increase cardiovascular risk.
Pregnancy can stress the female body significantly, acting as a “cardiac stress test” that reveals existing predispositions to cardiovascular disease (CVD) before traditional risk factors appear, according to a 2023 study. The American Heart Association calls pregnancy a “period of potential vulnerability,” which may increase the risk of developing a CVD in the future.
Pregnancy complications also heighten cardiovascular risks. Women who experience preeclampsia, preterm delivery, pregnancy loss, or gestational diabetes face higher rates of CVD compared to those without these complications.
READ MORE: What Happens to Your Body During Pregnancy, According to Oura Member Data
5. Women are more likely to have autoimmune conditions than can increase cardiovascular risk.
Women are more prone to autoimmune disease; in fact, women have up to a fourfold increase in autoimmune risk compared to men. For women who are diagnosed with autoimmune conditions like rheumatoid arthritis or lupus, there’s an associated increased risk for heart disease.
6. The female heart is more vulnerable to mental or emotional stress.
While mental stress can take a toll on anyone, research suggests that the female heart is more drastically affected by stress than the male heart.
In a recent study, researchers found that women under stressful conditions experience more constricting and tightening of their small peripheral arteries (the blood vessels that carry blood from the heart to the rest of the body) than men under the same stress.
That’s perhaps why women are more likely to experience Takotsubo syndrome, also known as “broken heart syndrome,” during bouts of extreme stress.
7. It’s possible for women to lower their risk.
Here’s the bright side: Heart disease in women can largely be prevented. In fact, research estimates that 80% of cardiovascular disease, including heart disease and stroke, can be prevented and even reversed through healthy behaviors.
Prevention begins with understanding. By staying informed about your heart health, making healthier lifestyle choices, and keeping up with your doctor’s appointments, women of any age can be more empowered to take control of their heart health.
RELATED: All About Cardiovascular Age
5 Tips to Lower Your Risk of Heart Disease

1. Know Your Stats
It can be helpful to monitor your heart rate using a wearable like Oura. The normal heart rate for women can be anywhere between 60 to 100 beats per minute (bpm). While slightly below this normal range, the average heart rate for female Oura members is 58 bpm.
2. Improve your diet.
Limit processed foods, sugar-sweetened beverages, and foods with high amounts of sugar, salt, and saturated fat. Instead, opt for a Mediterranean-style diet rich in plant foods, fish, and healthy fats.
3. Exercise regularly.
Aim for at least 150 minutes of medium-intensity aerobic physical activity or 75 to 150 minutes of high-intensity aerobic physical activity per week. Add in some strength training at a medium or high intensity two or more days per week.
4. Reduce tobacco and alcohol use.
Smoking is a major cause of cardiovascular disease — women who smoke have a 25% increased risk of developing heart disease compared to men who smoke. Alcohol consumption similarly impacts heart health, so it’s best to moderate or eliminate both.
5. Manage stress.
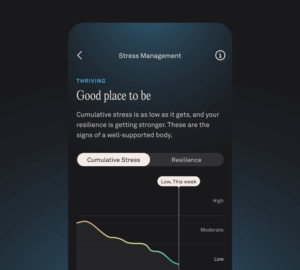
While it’s easier said than done, try to keep your stress levels in check with high-quality sleep, adequate exercise, breathwork or meditation, and staying socially connected.
READ MORE: How to Improve Your Cardiovascular Health