As we age, changes become apparent in our health, from our sleeping patterns to our heart health. To explore these shifts, members of Oura’s Science Team conducted two studies that analyzed aggregated, de-identified data from over 25,000 Oura members.
Led by Oura scientists Iman Alikhani, PhD, Mari Karsikas, PhD, and Max de Zambotti, PhD, these two studies reveal how aging impacts sleep duration, sleep architecture (the composition and progression of sleep stages and sleep cycles), circadian rhythm, and how these patterns differ between males and females. Plus, they shed light on how your sleep and physical activity directly influence two crucial health markers: resting heart rate (RHR) and heart rate variability (HRV).
Below, read the key takeaways from the analyses of sleep and heart health data—and what you can do now to sleep well and stay heart-healthy, no matter your age.
RELATED: How Sleeping Heart Rate Varies By Age
How Sleep Patterns Evolve with Age: Key Findings
Sleep Duration Declines Significantly
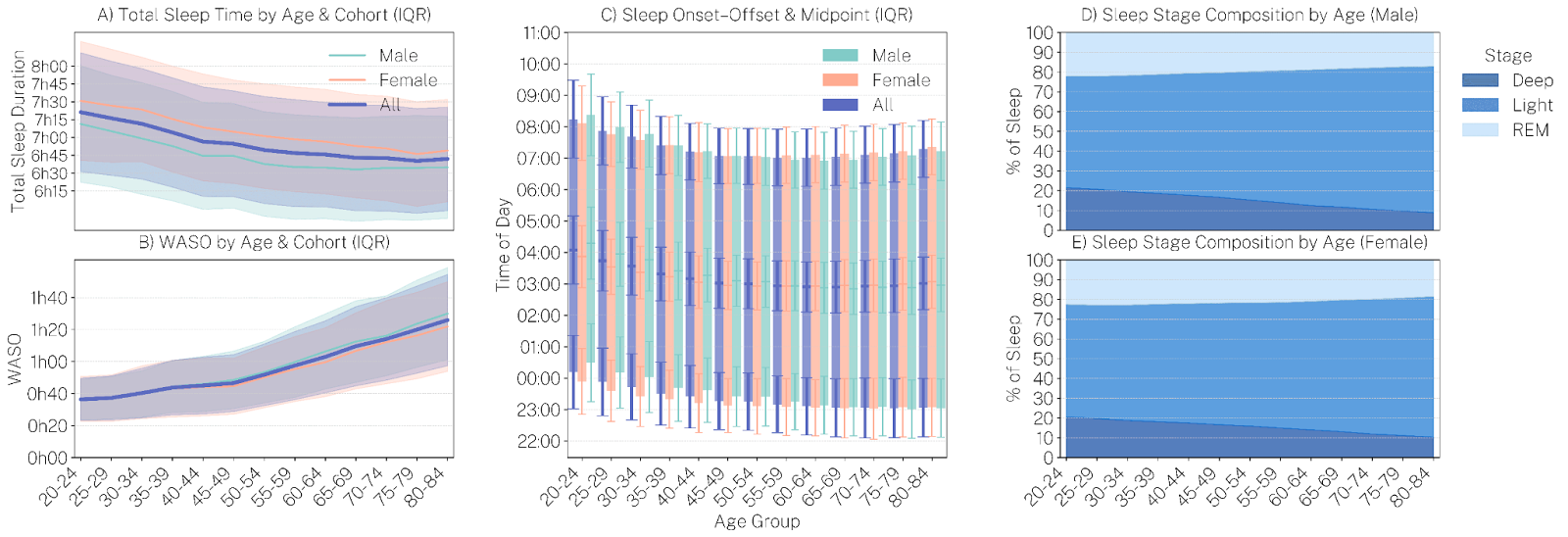
- Shortened sleep duration: Sleep duration gradually decreased with age, from an average of 7 hours 21 minutes (441 ± 78 minutes) among Oura members aged 20–25 to 6 hours 43 minutes (403 ± 68 minutes) by ages 80–85.
- Early to bed, early to rise: Sleep timing consistently shifted earlier with age, indicating a natural progression toward earlier bedtimes and wake times.
- As people age, they tend to spend more time awake during the night. Among the youngest group, WASO (Wake After Sleep Onset) was under 40 minutes, but this increased to over 1 hour and 20 minutes in the oldest age group.
- Gender differences: Across all age groups, women slept an average of 16.2 minutes longer than men.
While some reduction in total sleep may be a natural part of aging, it’s a powerful reminder to prioritize sleep hygiene to avoid detrimental effects on your health.
The finding that women sleep longer than men also aligns with previous research, and may be due to hormonal differences, reproductive demands, or variations in sleep architecture that increase the need for sleep.
LEARN MORE: Male and Female Sleep Patterns: How Do They Differ, and Why?
Deep & REM Sleep Decline, Light Sleep Dominates
- A decrease in deep sleep: Deep sleep declined by 50% from the 20-25-year-old group to the 80-85-year-old group.
- REM dips, but not as much: REM sleep began declining after age 35, with smaller decreases.
- Light sleep takes over: In the oldest age group, light sleep significantly increased to comprise 70–75% of total sleep.
Sleep architecture refers to how you cycle through different stages of sleep. Ideally, adults spend about 2–5% of their sleep time awake, 45–55% in light sleep, 13–23% in deep sleep, and 20–25% in REM sleep.
Both biological (e.g., hormonal changes) and environmental (e.g., light exposure) factors can influence sleep architecture. But the consistent, progressive trends in this dataset suggest that age-related biological shifts are the primary drivers of these changes.
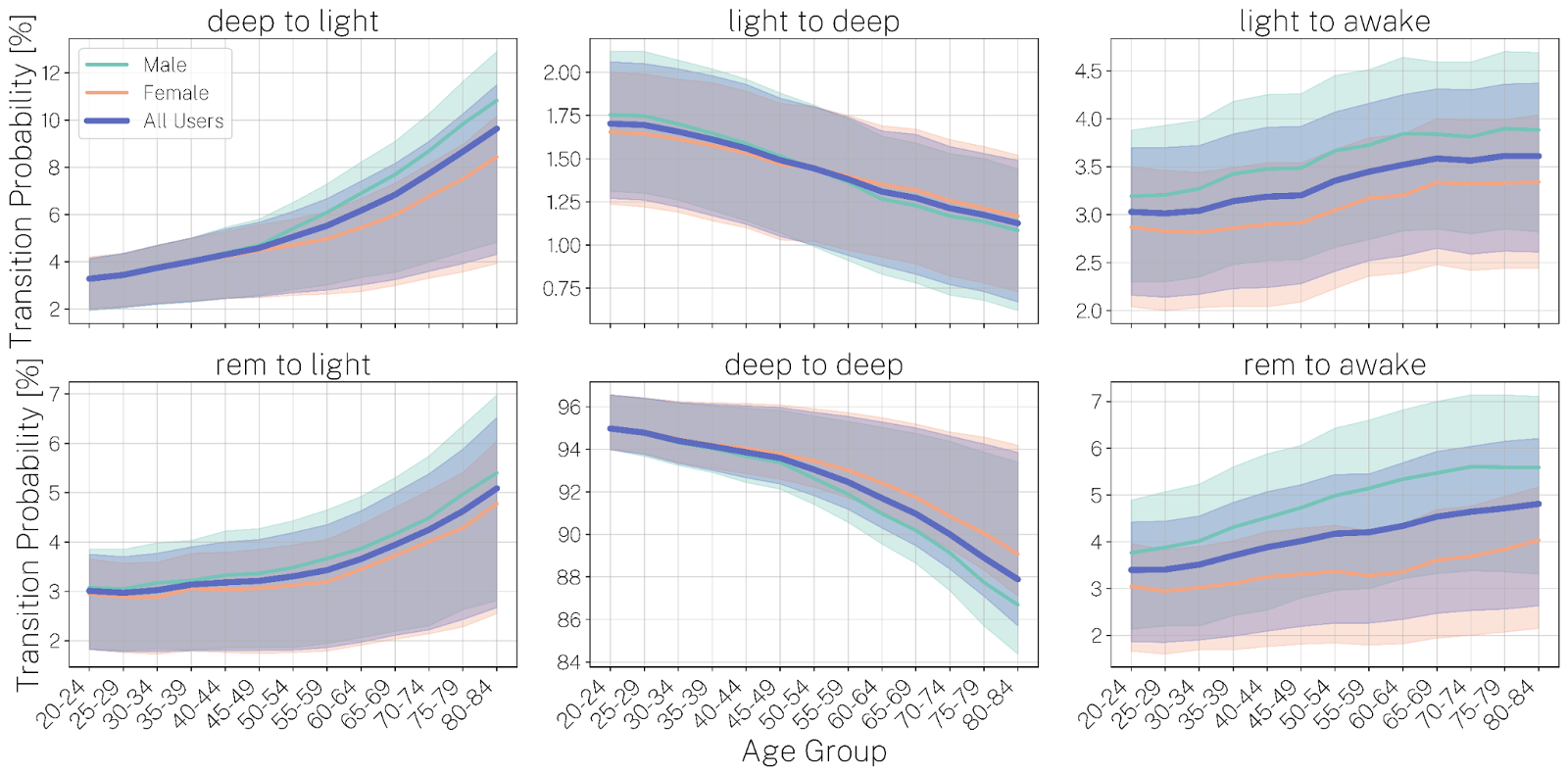
Sleep stage transition assessments show how often a person moves between different sleep stages (like light, deep, REM, and wake) throughout the night. It’s used to understand sleep continuity and fragmentation, helping researchers and clinicians assess sleep quality and identify patterns linked to age, health, or sleep disorders.
- The number of transitions from sleep stages to awake (e.g., REM to Wake, Light to Wake) increases steadily with age, indicating more fragmented and less consolidated sleep in older adults. This aligns with increased WASO and lighter overall sleep.
- Some transitions, particularly into REM and deep sleep, decrease with age, which reflects a diminished ability to enter or maintain restorative sleep stages.
READ MORE: How Your Sleep Needs Change Throughout Your Life
How Heart Health Changes with Age: Key Findings
In a complementary analysis of 25,759 Oura members (ages 20–85, balanced by sex), our researchers uncovered clear biological trends in sleep-related heart metrics.
Resting Heart Rate (RHR)
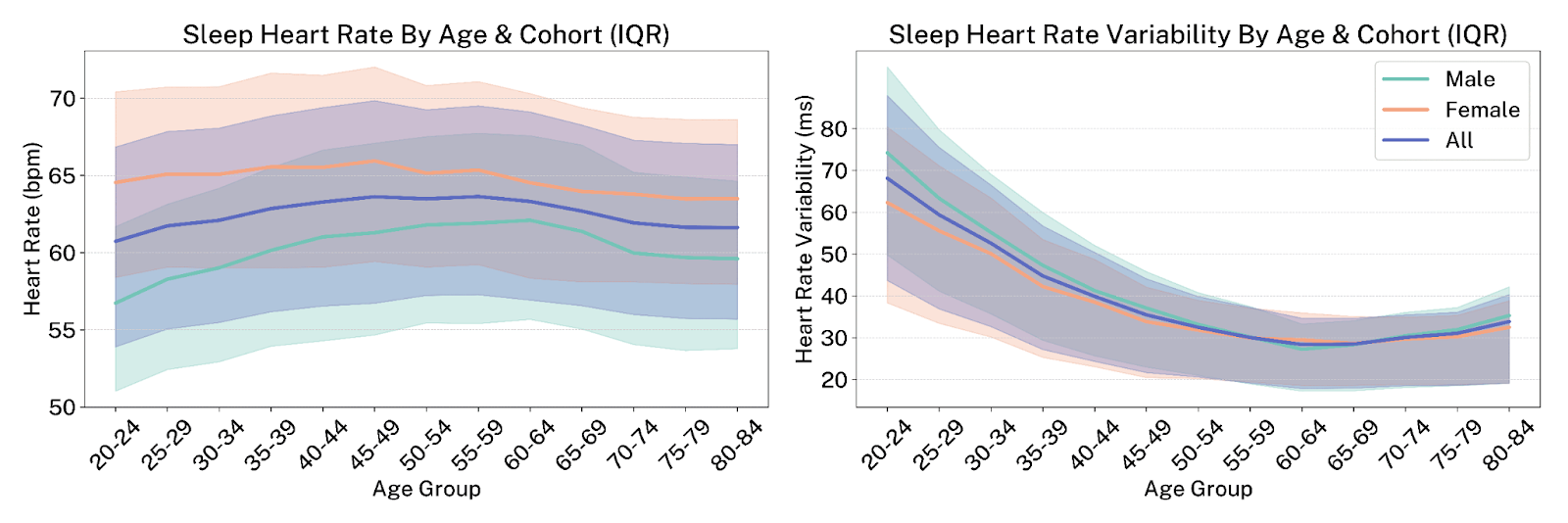
- Women had a consistently higher RHR compared to men, by 7.5 bpm on average in the youngest age group, narrowing to around 5 bpm in older adults.
- RHR peaked above 65 bpm for women in their forties and early fifties, whereas for men, it peaks around 62 bpm later in their fifties and early sixties.
Heart Rate Variability (HRV)
- HRV followed an asymmetric U-shaped pattern—generally declining from early life to mid-adulthood and then slightly increasing in older age.
- Women had lower HRV values than men in early to mid-adulthood (ages 20–44), even with their longer sleep durations.
LEARN MORE: How To Improve Your HRV (Heart Rate Variability)
Beyond the Numbers: How Sleep & Activity Influence Your Heart Health
These studies also found that lifestyle factors play a significant role in heart-health metrics such as RHR and HRV, regardless of your age.
- Short sleep & low activity: Short sleep (less than 6 hours) and low physical activity level (less than 5,000 steps/day) were consistently linked to higher RHR and lower HRV.
- Longer sleep & high activity: In contrast, longer sleep duration and higher physical activity level (more than 12,500 steps/day) correlated with lower RHR and higher HRV.
The takeaway? These ”dose-dependent” relationships held true across all age groups and both sexes. This means that proactive habits like consistent sleep and regular movement can significantly impact your heart health, offering a powerful tool for resilience as you age.
RELATED: Oura Member Data Reveals Gender Differences in Sleep, Stress, and Activity Levels











