During menopause, significant hormonal fluctuations occur throughout your body, triggering a cascade of changes, from shifts in mood and muscle loss to disruptions in how your body processes blood sugar. Consequently, these shifts can directly affect metabolic health, particularly concerning insulin resistance and sustained weight management.
Discover the effects of menopause on insulin sensitivity, plus explore strategies to optimize your metabolic health and overall wellbeing during this life stage.
RELATED: What Is Metabolic Health? A Comprehensive Guide
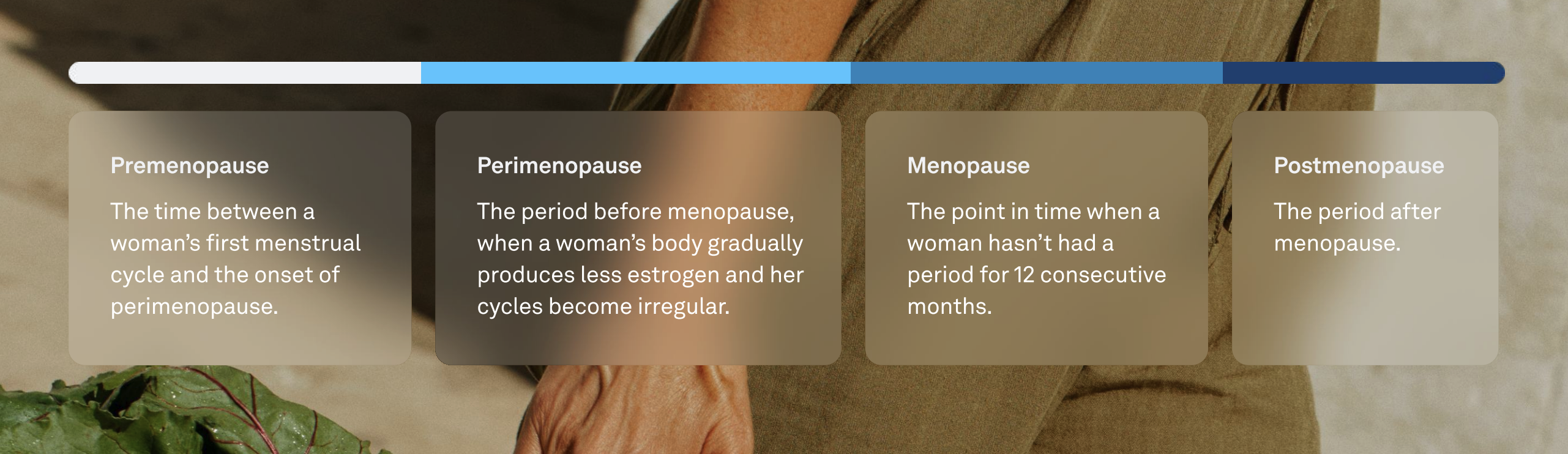
Menopause: A Natural Biological Transition
Menopause, which occurs on average at age 52 in the U.S., signifies the natural end of a woman’s reproductive years. This transition involves a gradual decline of progesterone levels due to less frequent ovulation, while estrogen levels fluctuate wildly with unpredictable highs and lows, causing a range of symptoms and increasingly irregular menstrual cycles before eventually settling at a consistently low level.
Alongside these reproductive changes, you may also experience symptoms like hot flashes, night sweats, mood swings, sleep disturbances, and changes in sexual function and memory.
This hormonal transition also influences your metabolic function. Declining estrogen can impact how your body regulates glucose, stores fat, and builds muscle—raising the risk of insulin resistance, weight gain, and cardiovascular disease.
The good news: Focusing on your nutritional choices, getting your body moving, and getting high-quality sleep helps support a healthy metabolism and feel your best through every stage of the transition.
READ MORE: How Oura Can Help You Manage Perimenopause
The Link Between Menopause and Insulin Resistance
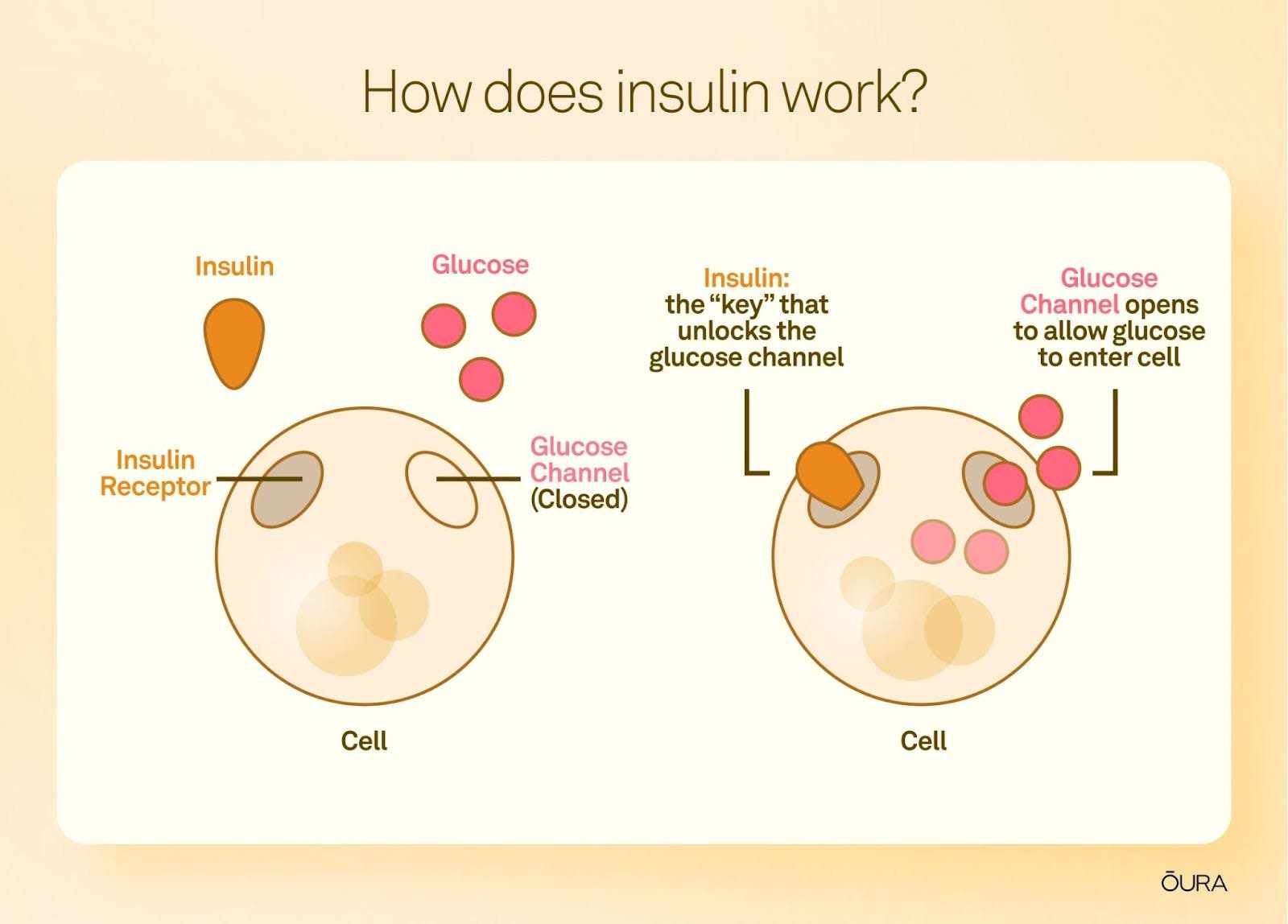
Estrogen helps your body regulate blood sugar by supporting insulin sensitivity. When estrogen declines, your body may become less responsive to insulin. That means glucose stays in your bloodstream longer—leading to elevated blood sugar and, over time, may lead to insulin resistance.
Other changes that can make it harder to maintain metabolic balance during menopause include:
- Muscle loss (sarcopenia): Muscle helps your body burn energy efficiently. Losing it can slow your metabolism and reduce insulin sensitivity.
- Fat redistribution: The body becomes more likely to store fat around the abdomen, which is strongly linked to metabolic dysfunction.
- Reduced physical activity: Lower energy, poor sleep, or joint pain may lead to more sedentary days—further impacting insulin and weight.
- PCOS history: If you’ve had polycystic ovarian syndrome (PCOS), you may already be more prone to insulin resistance, making menopausal changes more significant.
Together, these shifts can increase your risk for type 2 diabetes, high blood pressure, and cardiovascular conditions if left unaddressed. But when they are addressed with small shifts in your daily habits, you can rebuild insulin sensitivity, support muscle mass, and keep your metabolism resilient through menopause and beyond.
How to Support Your Metabolic Health During Menopause
Your metabolism doesn’t have to take a backseat during menopause. These lifestyle strategies can help you stay balanced and reduce the risk of long-term complications:
1. Prioritize Sleep
Declining hormone levels can disrupt sleep—especially if hot flashes or anxiety kick in at night. Aim for 7–9 hours of quality sleep and keep a consistent bedtime to support glucose metabolism and recovery.
READ MORE: How Does Menopause Affect Sleep?
2. Move Your Body Regularly
Exercise is one of the most effective ways to maintain muscle mass, boost insulin sensitivity, and improve mood and sleep. Aim for:
- 150 minutes of moderate cardio (e.g. brisk walking, cycling) or 75 minutes of vigorous cardio per week
- At least two strength-training sessions per week
| Member Tip: Oura automatically tracks all of your movement. Whether it’s housework, a walk, or pickleball—it all counts towards your Activity Goal. |
3. Eat for Blood Sugar Balance
Build meals with protein, fiber, and healthy fats. Cut back on refined sugars and ultra-processed foods that spike your glucose. Think: colorful veggies, lean meats or fish, legumes, and omega-3s from nuts or seeds.
For added benefit, try sequence eating—starting your meal with fiber-rich vegetables, then protein and fats, and saving carbohydrates for last—which has been shown to reduce post-meal glucose spikes and improve insulin response.
READ MORE: The Essential Guide to Eating for Optimal Metabolic Health
4. Manage Stress
Chronic stress raises cortisol, which can increase blood sugar and reduce insulin sensitivity. Try breathing exercises, gentle movement, or meditation to lower daily stress loads and protect your heart.
| Member Tip: Access guided breathing exercises and meditations on the Oura App under Explore content. |
5. Limit Smoking and Alcohol
Both can interfere with sleep, glucose regulation, and hormone balance. Cutting back on alcohol and avoiding smoking can support healthier aging and metabolic resilience.
| Member Story: Oura member Gemma R. quit drinki ng alcohol and noticed an improvement in her resting heart rate, from 90 bpm to 55. |
6. Consider Hormone Therapy—If It’s Right for You
While lifestyle changes are foundational, they may not fully resolve symptoms for everyone. For some, hormone replacement therapy (HRT) can ease symptoms and improve metabolic markers. Talk with a healthcare provider to see if it’s a safe and beneficial option for your needs.
7. Keep Portions in Check
Your metabolic rate may slow slightly during and after menopause, so consider discussing your caloric needs with your healthcare provider to ensure you are eating in alignment with your needs. Portion awareness can help prevent unintentional weight gain and keep glucose levels in range.
RELATED: The Surprising Link Between Menopause and Sleep Apnea