Wearable sleep trackers are gaining users rapidly around the world, offering unprecedented insights into your nightly rest. Yet until recently, guidance on how to use and interpret their data has been focused on technical details and shortcomings rather than what these devices can and cannot yet do in real-world settings.
A new set of recommendations from the World Sleep Society Sleep Tracker Task Force was published in Sleep Medicine, bringing clarity and pragmatic guidance for consumers, clinicians, and researchers alike.
The report advocates for standardized fundamental sleep measures, best practices for device selection, and steps toward integrating wearable data into clinical records.
The Need for Better Sleep Tracker Guidance
“Health trackers have tremendous potential to benefit human health, offering a more comprehensive picture of sleep,“ says lead author, Michael Chee, MBBS, FRCP(Edin), Director of the Centre for Sleep and Cognition at the National University of Singapore, and Oura Advisor.
Current sleep guidelines are heavily based on self-reported data, and are drawn almost entirely from North American and European studies (just 15% of the world’s population). This means the data may not be representative of diverse populations, overlooking cultural, demographic, and lifestyle differences in sleep patterns.
“Wearables have the potential to fill this gap in our understanding of sleep, collecting long-term, diverse data and providing up-to-date, demographic-tailored advice,” says Chee. “However, currently, consumer enthusiasts and social media influencers guide public perceptions about sleep trackers more so than clinicians or sleep scientists.” This is why, according to Chee, these recommendations are needed.
READ MORE: Oura’s New Sleep Staging Algorithm: More Accurate Than Ever Before
How the Recommendations Were Developed
This guidance involved contributions from experts from leading sleep research centers in Asia, Europe, Australia, and North America, combining current literature, performance-evaluation frameworks, and the collective clinical experience of task force members.
The process involved:
- Literature synthesis summarizing knowledge about sensor technology, the physiology underlying sleep measurement using wearables, and the current responsible usage of wearables in three clinical settings.
- Definition of fundamental sleep measures (FSMs) to encourage harmonization of terminology across devices and sleep experts.
- Development of actionable recommendations for four stakeholder groups—end-users, healthcare professionals, researchers, and manufacturers—covering everything from bedtime detection to medical‐grade certification.
- Performance evaluation blueprint, detailing epoch-by-epoch analyses, Bland-Altman plots, and equivalence testing to benchmark wearable outputs against polysomnography.
The Core Sleep Metrics Your Sleep Tracker Should Have
To build a reliable foundation, the Task Force defines seven Fundamental Sleep Measures (FSMs) that every wearable should report in a clear, standardized format—complete with validation-study details and precision metrics—so you can confidently compare data across brands and over time. The core metrics include:
- Sleep onset: The period of time it takes for a person to transition from being fully awake to falling asleep
- Sleep offset: The time when sleep ends, marking the transition from sleeping to being awake
- Sleep latency: The time it takes to fall asleep after going to bed
- Total sleep time
- Wake after sleep onset (WASO): The duration of time spent awake during a sleep period after initially falling asleep
- Sleep efficiency: The percentage of time spent asleep while in bed
- Duration in light, deep, and REM sleep
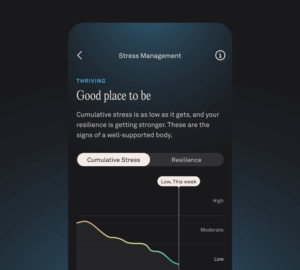
Beyond these essentials, many devices—including Oura Ring—offer additional, exploratory measures, such as sleep regularity, composite “Sleep Scores,” heart rate variability (HRV), respiratory rate, blood-oxygen levels, and breathing-disturbance alerts, which can enrich your understanding of sleep health.
READ MORE: How Does the Oura Ring Track My Sleep?
The Power of Sleep Wearables
The Task Force concludes that by anchoring wearable outputs to seven standardized sleep measures and acknowledging the limitations of wearables when evaluating persons with sleep disorders, consumer trackers can deliver reliable, long-term sleep data that can be significantly more valuable than single‐night lab studies.
For healthy users, they illuminate how daily routines impact rest; for those with insomnia or suspected sleep-disordered breathing, multi-night trends and breathing-disturbance alerts can prompt earlier clinical evaluation; and for researchers and clinicians, validated wearable metrics offer a scalable, at-home complement to polysomnography.
“While wearables cannot yet replace lab-based evaluation for persons with sleep disorders, they provide copious amounts of valuable information about how we sleep that can be related to what affects our sleep and the benefits of good sleep,” says Chee. “With ongoing validation studies and shared data standards, high-quality wearables will become an essential tool for personalizing sleep health in the majority of people. The future of sleep science is exciting.”